Regulatory Information
HSA regulatory responsibility and product classification details
Regulatory Responsibility
Product Classification
Formulation Information
INFUSION, SOLUTION CONCENTRATE
**DOSAGE AND ADMINISTRATION:** Pemetrexed Kabi must only be administered under the supervision of a physician qualified in the use of anti-cancer chemotherapy. Posology _Pemetrexed Kabi in combination with cisplatin_ The recommended dose of Pemetrexed Kabi is 500 mg/m2 of body surface area (BSA) administered as an intravenous infusion over 10 minutes on the first day of each 21-day cycle. The recommended dose of cisplatin is 75 mg/m2 BSA infused over two hours approximately 30 minutes after completion of the pemetrexed infusion on the first day of each 21-day cycle. Patients must receive adequate anti-emetic treatment and appropriate hydration prior to and/or after receiving cisplatin. _Pemetrexed Kabi in combination with pembrolizumab and platinum chemotherapy_ The recommended dose of Pemetrexed Kabi when administered with pembrolizumab and platinum chemotherapy for the initial treatment of metastatic non-squamous NSCLC in patients with a creatinine clearance (calculated by Cockcroft-Gault equation) of 45 mL/min or greater is 500 mg/m2 as an intravenous infusion over 10 minutes administered after pembrolizumab and prior to carboplatin or cisplatin on Day 1 of each 21-day cycle for 4 cycles. Following completion of platinum-based therapy, treatment with Pemetrexed Kabi with or without pembrolizumab is administered until disease progression or unacceptable toxicity. Please refer to the full prescribing information for pembrolizumab and for carboplatin or cisplatin. _Pemetrexed Kabi as single agent_ In patients treated for non-small cell lung cancer after prior chemotherapy, the recommended dose of Pemetrexed Kabi is 500 mg/m2 BSA administered as an intravenous infusion over 10 minutes on the first day of each 21-day cycle. _Pre-medication regimen_ To reduce the incidence and severity of skin reactions, a corticosteroid should be given the day prior to, on the day of, and the day after pemetrexed administration. The corticosteroid should be equivalent to 4 mg of dexamethasone administered orally twice a day. To reduce toxicity, patients treated with pemetrexed must also receive vitamin supplementation. Patients must take oral folic acid or a multivitamin containing folic acid (350 to 1000 micrograms) on a daily basis. The most commonly used dose of oral folic acid in clinical trials was 400mcg. At least five doses of folic acid must be taken during the seven days preceding the first dose of pemetrexed, and dosing must continue during the full course of therapy and for 21 days after the last dose of pemetrexed. Patients must also receive an intramuscular injection of vitamin B12 (1000 micrograms) in the week preceding the first dose of pemetrexed and once every three cycles thereafter. Subsequent vitamin B12 injections may be given on the same day as pemetrexed. _Monitoring_ Patients receiving pemetrexed should be monitored before each dose with a complete blood count, including a differential white cell count (WCC) and platelet count. Prior to each chemotherapy administration blood chemistry tests should be collected to evaluate renal and hepatic function. Before the start of any cycle of chemotherapy, patients are required to have the following: absolute neutrophil count (ANC) should be ≥ 1500 cells/mm3 and platelets should be ≥ 100,000 cells/mm3. Creatinine clearance should be ≥ 45 ml/min. The total bilirubin should be ≤ 1.5 times upper limit of normal. Alkaline phosphatase (AP), aspartate aminotransferase (AST or SGOT) and alanine aminotransferase (ALT or SGPT) should be ≤ 3 times upper limit of normal. Alkaline phosphatase, AST and ALT ≤ 5 times upper limit of normal is acceptable if liver has tumour involvement. _Dose adjustments_ Dose adjustments at the start of a subsequent cycle should be based on nadir haematologic counts or maximum non-haematologic toxicity from the preceding cycle of therapy. Treatment may be delayed to allow sufficient time for recovery. Upon recovery patients should be retreated using the guidelines in Tables 6, 7 and 8, which are applicable for Pemetrexed Kabi used as a single agent or in combination with cisplatin. 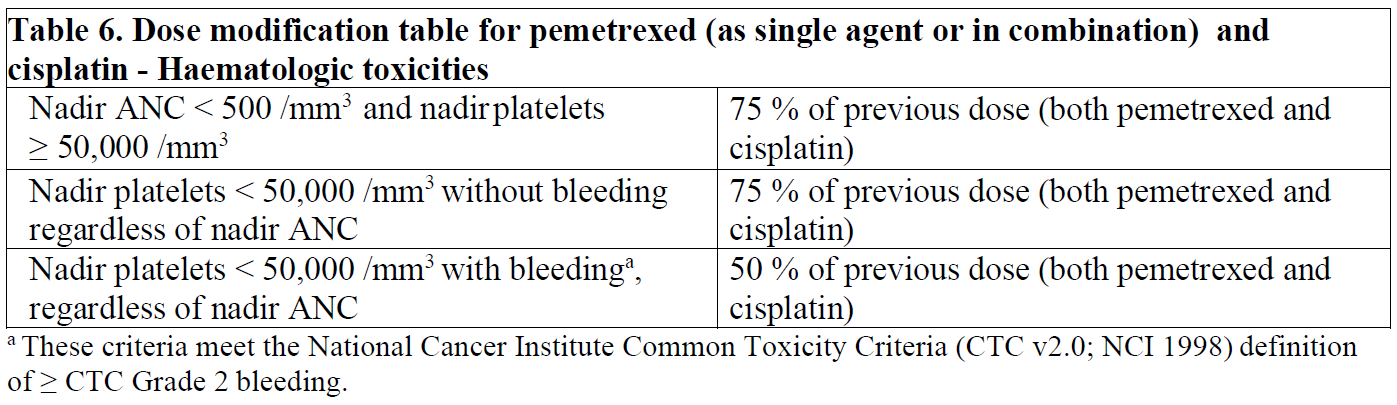 If patients develop non-haematologic toxicities ≥ Grade 3 (excluding neurotoxicity), Pemetrexed Kabi should be withheld until resolution to less than or equal to the patient’s pre-therapy value. Treatment should be resumed according to the guidelines in Table 7. 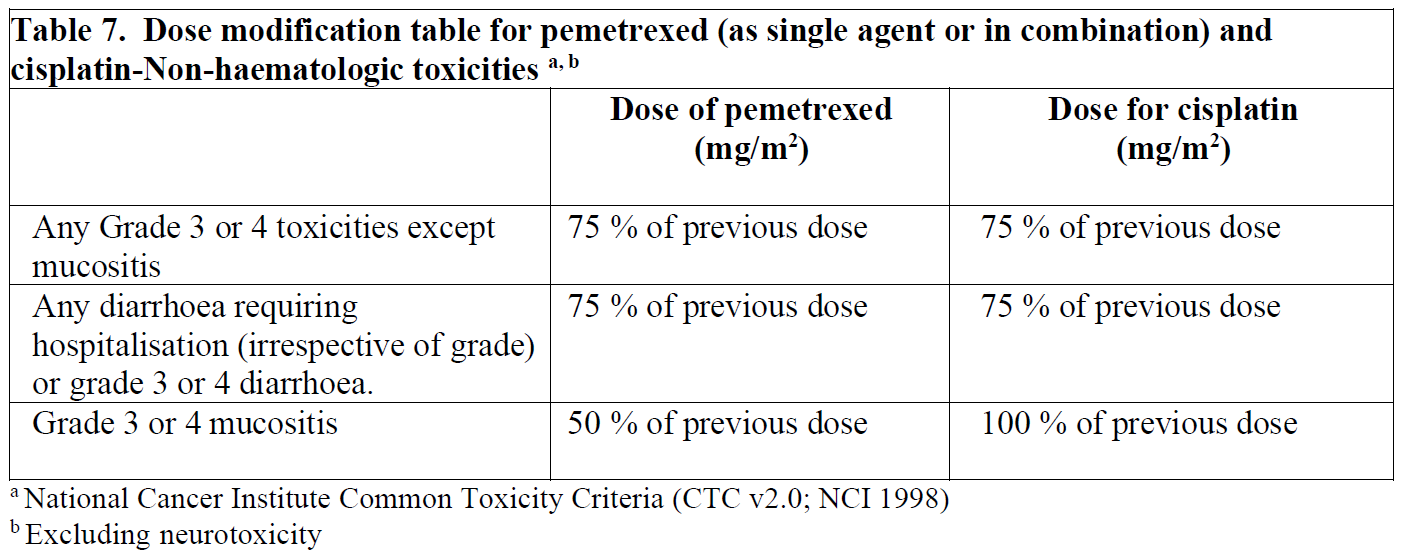 In the event of neurotoxicity, the recommended dose adjustment for Pemetrexed Kabi and cisplatin is documented in Table 8. Patients should discontinue therapy if Grade 3 or 4 neurotoxicity is observed. 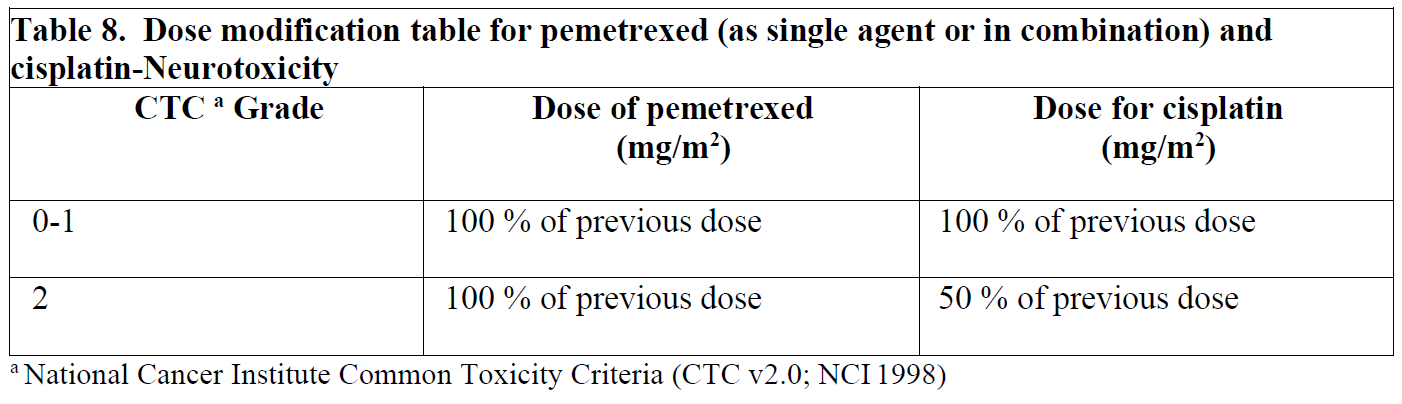 Treatment with Pemetrexed Kabi should be discontinued if a patient experiences any haematologic or non-haematologic Grade 3 or 4 toxicity after 2 dose reductions or immediately if Grade 3 or 4 neurotoxicity is observed. _Special populations_ _Elderly_ In clinical studies, there has been no indication that patients 65 years of age or older are at increased risk of adverse reaction compared to patients younger than 65 years old. No dose reductions other than those recommended for all patients are necessary. _Paediatric population_ Pemetrexed Kabi is not recommended for use in children below 18 years of age, due to insufficient data on safety and efficacy. _Patients with renal impairment (Standard Cockcroft and Gault formula or glomerular filtration rate measured Tc99m-DPTA serum clearance method)_ Pemetrexed is primarily eliminated unchanged by renal excretion. In clinical studies, patients with creatinine clearance of ≥ 45 ml/min required no dose adjustments other than those recommended for all patients. There are insufficient data on the use of pemetrexed in patients with creatinine clearance below 45 ml/min; therefore, the use of pemetrexed is not recommended. _Patients with hepatic impairment_ No relationships between AST (SGOT), ALT (SGPT), or total bilirubin and pemetrexed pharmacokinetics were identified. However, patients with hepatic impairment such as bilirubin > 1.5 times the upper limit of normal and/or aminotransferase > 3.0 times the upper limit of normal (hepatic metastases absent) or > 5.0 times the upper limit of normal (hepatic metastases present) have not been specifically studied. Method of administration Pemetrexed Kabi is for intravenous use. Pemetrexed Kabi should be administered as an intravenous infusion over 10 minutes on the first day of each 21-day cycle. - Use aseptic technique during the dilution of pemetrexed for intravenous infusion administration. - Calculate the dose and the number of Pemetrexed Kabi vials needed. - The appropriate volume of Pemetrexed Kabi must be diluted to 100 ml with sodium chloride 9 mg/ml (0.9 %) solution for injection or 5% glucose intravenous infusion and administered as an intravenous infusion over 10 minutes. - Pemetrexed infusion solutions prepared as directed above are compatible with polyvinyl chloride and polyolefin lined administration sets and infusion bags. - Parenteral medicinal products must be inspected visually for particulate matter and discolouration prior to administration. If particulate matter is observed, do not administer. - Pemetrexed solutions are for single use only. Any unused medicinal product or waste material must be disposed of in accordance with local requirements.
INTRAVENOUS
Medical Information
**INDICATIONS:** Malignant Pleural Mesothelioma (MPM): Pemetrexed Kabi in combination with cisplatin is indicated for the treatment of chemotherapy naïve patients with unresectable MPM or who are otherwise not candidates for curative surgery. Non-Small Cell Lung Cancer (NSCLC): Pemetrexed Kabi in combination with cisplatin is indicated for the first line treatment of patients with locally advanced or metastatic non-squamous NSCLC. Pemetrexed Kabi in combination with pembrolizumab, and platinum chemotherapy, is indicated for the first-line treatment of patients with metastatic non-squamous NSCLC, with no EGFR or ALK genomic tumor aberrations. Pemetrexed Kabi is indicated as monotherapy for the maintenance treatment of locally advanced or metastatic non-squamous NSCLC in patients whose disease has not progressed immediately following first-line treatment with platinum-based chemotherapy. Pemetrexed Kabi is indicated as monotherapy for the second line treatment of patients with locally advanced or metastatic non-squamous NSCLC.
**CONTRAINDICATIONS:** Hypersensitivity to the active substance or to any of the excipients. Breast feeding. Concomitant yellow fever vaccine.
L01BA04
pemetrexed
Manufacturer Information
FRESENIUS KABI (SINGAPORE) PTE LTD
Fresenius Kabi Oncology Limited
Active Ingredients
Documents
Package Inserts
Pemetrexed Kabi Concentrate for Solution for Infusion 25mg per ml PI.pdf
Approved: July 3, 2023
