Regulatory Information
HSA regulatory responsibility and product classification details
Regulatory Responsibility
Product Classification
Formulation Information
INJECTION, SOLUTION
**Posology and method of administration** Posology **ADULTS** **Rheumatoid Arthritis, Psoriatic Arthritis and Ankylosing Spondylitis** The recommended dose of Adalimumab for adult patients with rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis is 40 mg administered every other week as a single dose via subcutaneous injection. Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory drugs, analgesics or other DMARDs may be continued during treatment with Adalimumab. In rheumatoid arthritis, some patients not taking concomitant MTX may derive additional benefit from increasing the dosage of adalimumab to 40 mg every week or 80 mg every other week. **Crohn’s Disease** 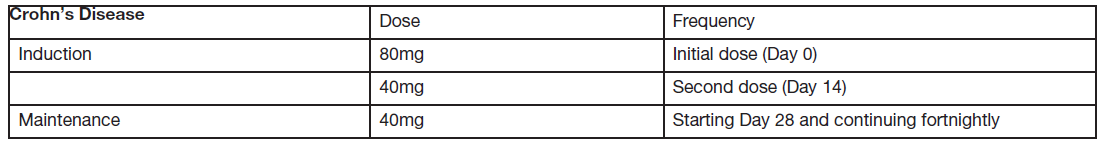 In case there is a need for a more rapid response to therapy, the regimen 160 mg at week 0 (given as 160 mg in one day or as 80 mg per day for two consecutive days), 80 mg at week 2, can be used with the awareness that the risk for adverse events is higher during induction. Some patients who experience a decrease in their response may benefit from an increase in dosage to 40 mg Adalimumab every week or 80mg every other week. Aminosalicylates, corticosteroids, and/or immunomodulatory agents (e.g., 6-mercaptopurine and azathioprine) may be continued during treatment with Adalimumab. Patients usually respond within the induction phase. However, if a patient does not show any response, available data do not sufficiently support further Adalimumab treatment. **Ulcerative Colitis** The recommended Adalimumab induction dose regimen for adult patients with moderate to severe ulcerative colitis is 160 mg at Week 0 (given as 160 mg in one day or as 80 mg per day for two consecutive days) and 80 mg at Week 2. After induction treatment, the recommended dose is 40 mg every other week via subcutaneous injection. Aminosalicylates, corticosteroids, and/or immunomodulatory agents (e.g., 6-mercaptopurine and azathioprine) may be continued during treatment with Adalimumab. During maintenance treatment, corticosteroids may be tapered in accordance with clinical practice guidelines. Some patients who experience decrease in their response may benefit from an increase in dosage to 40 mg Adalimumab every week or 80 mg every other week. Available data suggest that clinical response is usually achieved within 2–8 weeks of treatment. Adalimumab should only be continued in patients who have responded during the first 8 weeks of therapy. **Plaque Psoriasis** The recommended dose of Adalimumab for adult patients with plaque psoriasis is an initial dose of 80 mg, followed by 40 mg given every other week starting one week after the initial dose. Continued therapy beyond 16 weeks should be carefully reconsidered in a patient not responding within this time period. Beyond 16 weeks, patients with inadequate response may benefit from an increase in dosage to 40 mg every week or 80 mg every other week. Response should be periodically evaluated (for example, every 12 weeks). Patients with continued inadequate response should discontinue treatment. If an adequate response is achieved with an increased dosage, the dose may subsequently be reduced to 40mg fortnightly. **Hidradenitis Suppurativa** The recommended Adalimumab dose regimen for adult patients with hidradenitis suppurativa (HS) is 160 mg initially at Day 1 (given as 160 mg in one day or as 80 mg per day for two consecutive days), followed by 80 mg two weeks later at Day 15. Two weeks later (Day 29) continue with a dose of 40 mg every week or 80 mg every other week. Antibiotics may be continued during treatment with Adalimumab if necessary. It is recommended that the patient should use a topical antiseptic wash on their HS lesions on a daily basis during treatment with Adalimumab. Should treatment need to be interrupted, Adalimumab 40 mg every week may be re-introduced. In patients without any benefit after 12 weeks of treatment, continued therapy should be reconsidered. **Uveitis** Ophthalmologists are advised to consult with an appropriate specialist before initiation of treatment with Adalimumab. The recommended dose of Adalimumab for adult patients with uveitis is an initial dose of 80 mg, followed by 40 mg given every other week starting one week after the initial dose. There is limited experience in the initiation of treatment with Adalimumab alone. Treatment with Adalimumab can be initiated in combination with corticosteroids and/or with other non-biologic immunomodulatory agents. Concomitant corticosteroids may be tapered in accordance with clinical practice starting two weeks after initiating treatment with Adalimumab. It is recommended that the benefit and risk of continued long-term treatment should be evaluated on a yearly basis. Paediatric population Hulio is only available as 40 mg pre-filled syringe and 40 mg pre-filled pen. It is not possible to administer Hulio to paediatric patients that require less than a full 40 mg dose. If a dose other than 40 mg is required, other adalimumab products offering such an option should be used. _Juvenile idiopathic arthritis_ Polyarticular Juvenile Idiopathic Arthritis The recommended dose of Adalimumab for patients from 2 years of age with polyarticular juvenile idiopathic arthritis (JIA) is based on body weight (Table 26). MTX, glucocorticoids, NSAIDs, and/or analgesics may be continued during treatment with Adalimumab. Adalimumab may be available in different strengths and/or presentations. 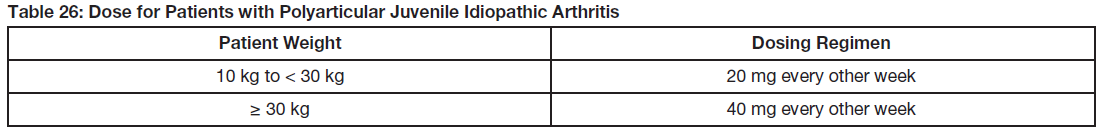 Adalimumab has not been studied in patients with polyarticular juvenile idiopathic arthritis less than 2 years of age or in patients with a weight below 10kg. Available data suggest that clinical response is usually achieved within 12 weeks of treatment. Continued therapy should be carefully reconsidered in a patient not responding within this time period. There is no relevant use of Adalimumab in children aged less than 2 years in this indication. _Enthesitis-related arthritis_ The recommended dose of Hulio for patients from 6 years of age with enthesitis-related arthritis is based on body weight (Table 27). Hulio may be available in different strengths and/or presentations. 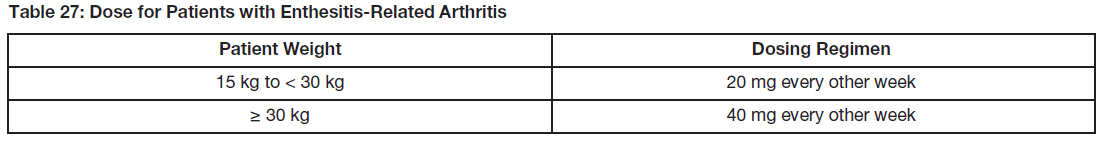 Adalimumab has not been studied in patients with enthesitis-related arthritis aged less than 6 years. _Paediatric plaque psoriasis_ The recommended Adalimumab dose for patients from 4 to 17 years of age with plaque psoriasis based on body weight (Table 28). Adalimumab is administered via subcutaneous injection. Adalimumab may be available in different strengths and/or presentations. 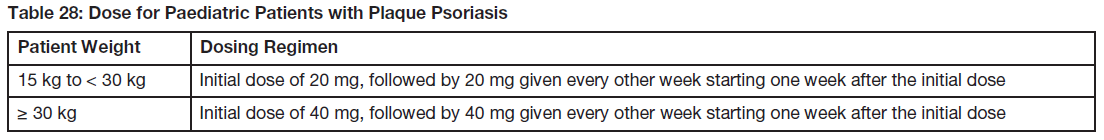 Continued therapy beyond 16 weeks should be carefully considered in a patient not responding within this time period. If retreatment with Adalimumab is indicated, the above guidance on dose and treatment duration should be followed. There is no relevant use of adalimumab in children aged less than 4 years for this indication. _Adolescent hidradenitis suppurativa_ There are no clinical trials with adalimumab in adolescent patients with hidradenitis suppurativa (HS). The posology of adalimumab in these patients has been determined from pharmacokinetic modelling and simulation. The recommended Adalimumab dose in adolescent patients from 12 years of age weighing at least 30 kg with hidradenitis suppurativa is 80 mg at week 0 followed by 40 mg every other week starting at week 1 via subcutaneous injection. Adalimumab may be available in different strengths and/or presentations. In adolescent patients with inadequate response to Adalimumab 40 mg every other week, an increase in dosage to 40 mg every week or 80 mg every other week may be considered. Antibiotics may be continued during treatment with Adalimumab if necessary. It is recommended that the patient should use a topical antiseptic wash on their HS lesions on a daily basis during treatment with Adalimumab. Continued therapy beyond 12 weeks should be carefully reconsidered in a patient with no improvement within this time period. Should treatment be interrupted, adalimumab may be re-introduced as appropriate. The benefit and risk of continued long-term treatment should be periodically evaluated. There is no relevant use of adalimumab in children aged less than 12 years in this indication. Adalimumab may be available in other presentations depending on the individual treatment needs. _Paediatric Crohn's disease_ The recommended dose of Adalimumab for patients from 6 to 17 years of age with Crohn’s disease is based on body weight (Table 29). Adalimumab is administered via subcutaneous injection. Adalimumab may be available in different strengths and/or presentations. 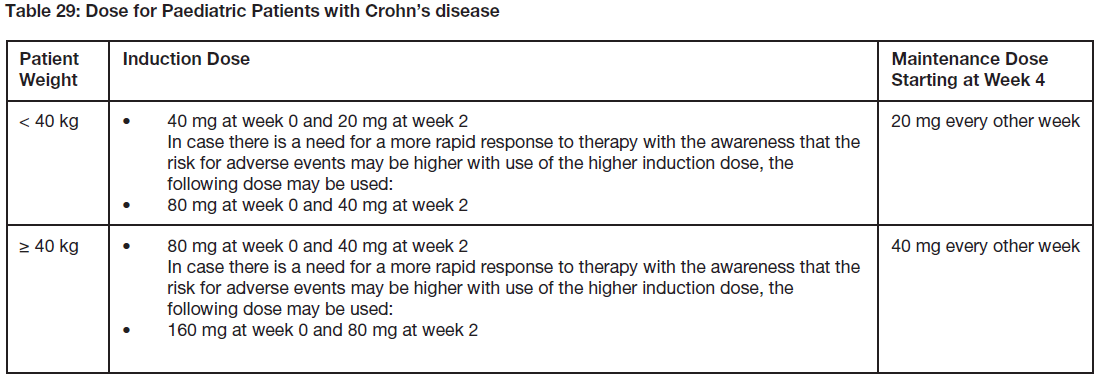 Patients who experience insufficient response may benefit from an increase in dosage: - _< 40 kg: 20 mg every week_ - _≥ 40 kg: 40 mg every week or 80 mg every other week_ Adalimumab has not been studied in children with Crohn’s disease aged less than 6 years. _Paediatric Uveitis_ The recommended dose of Adalimumab for paediatric patients 2 years of age and older with chronic non-infectious anterior uveitis is based on body weight (Table 30). Adalimumab is administered via subcutaneous injection. Adalimumab may be available in different strengths and/or presentations. In paediatric uveitis, there is no experience in the treatment with Adalimumab without concomitant treatment with methotrexate. 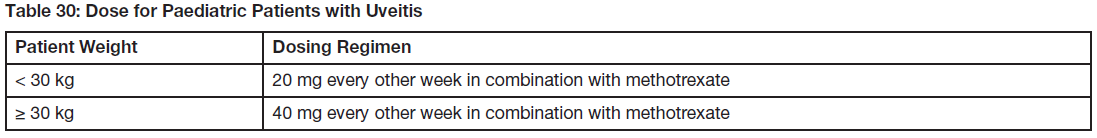 When Adalimumab therapy is initiated, a loading dose of 40 mg for patients < 30 kg or 80 mg for patients ≥ 30 kg may be administered one week prior to the start of maintenance therapy. No clinical data are available on the use of a Adalimumab loading dose in children < 6 years of age. There is no relevant use of adalimumab in children aged less than 2 years in this indication. It is recommended that the benefit and risk of continued long-term treatment should be evaluated on a yearly basis. **Pediatric Use** Adalimumab has not been studied in children less than 2 years of age and there are limited data on Hulio treatment in children with weight < 10kg. The safety and efficacy of Adalimumab in pediatric patients for indications other than juvenile idiopathic arthritis (polyarticular juvenile idiopathic arthritis and enthesitis-related arthritis), pediatric Crohn’s disease, pediatric plaque psoriasis, adolescent hidradenitis suppurativa and pediatric uveitis have not been established. **Geriatric Use** Of the total number of subjects in clinical studies of Hulio, 9.4% were 65 years and over, while approximately 2.0% were 75 and over. No overall differences in effectiveness were observed between these subjects and younger subjects. No dose adjustment is needed for this population. Method of administration Hulio is administered by subcutaneous injection.
SUBCUTANEOUS
Medical Information
**Therapeutic indications** **ADULTS** **Rheumatoid Arthritis** Hulio is indicated for reducing signs and symptoms and inhibiting the progression of structural damage and improving physical function in adult patients with moderately to severely active rheumatoid arthritis who have had an inadequate response to one or more DMARDs. Hulio can be used alone or in combination with methotrexate or other DMARDs. Hulio, in combination with MTX, can also be used in the treatment of patients with recently diagnosed moderate to severely active rheumatoid arthritis who have not received methotrexate. **Psoriatic Arthritis** Hulio is indicated for reducing signs and symptoms of active arthritis in adult patients with moderate to severe psoriatic arthritis when the response to previous DMARD therapy has been inadequate. Hulio has been shown to reduce the rate of progression of peripheral joint damage as measured by X-ray in patients with polyarticular symmetrical subtypes of the disease and to improve physical function. Hulio can be used alone or in combination with DMARDs. **Ankylosing Spondylitis** Hulio is indicated for reducing signs and symptoms in adult patients with active ankylosing spondylitis who have had an inadequate response to conventional therapy. **Crohn’s Disease** Hulio is indicated for the treatment of moderate to severe active Crohn’s disease in adults to reduce the signs and symptoms of the disease and to induce and maintain clinical remission in patients who have had an inadequate response to conventional therapies, or who have lost response to or are intolerant of infliximab. For induction treatment, Hulio should be given in combination with corticosteroids. Hulio can be given as monotherapy in case of intolerance to corticosteroids or when continued treatment with corticosteroids is inadequate. **Ulcerative Colitis** Hulio is indicated for treatment of moderately to severely active ulcerative colitis in adult patients who have had an inadequate response to conventional therapy including corticosteroids and/or 6-mercaptopurine (6-MP) or azathioprine (AZA), or who are intolerant to or have medical contraindications for such therapies. **Plaque Psoriasis** Hulio is indicated for the treatment of adult patients with moderate to severe chronic plaque psoriasis who are candidates for systemic therapy or phototherapy and when other systemic therapies are medically less appropriate. **Hidradenitis Suppurativa** Hulio is indicated for the treatment of active moderate to severe hidradenitis suppurativa (acneinversa) in adult patients with an inadequate response to conventional systemic HS therapy. **Uveitis** Hulio is indicated for the treatment of non-infectious intermediate, posterior and panuveitis in adult patients who have had an inadequate response to corticosteroids, in patients in need of corticosteroid-sparing, or in whom corticosteroid treatment is inappropriate. **PEDIATRICS** **Juvenile Idiopathic Arthritis** **_Polyarticular Juvenile Idiopathic Arthritis_** Hulio in combination with methotrexate is indicated for the treatment of active polyarticular juvenile idiopathic arthritis (pJIA), in patients 2 years of age and older, who have had an inadequate response to one or more disease-modifying anti-rheumatic drugs (DMARDS). Hulio can be given as monotherapy in case of intolerance to methotrexate or when continued treatment with methotrexate is inappropriate (for the efficacy in monotherapy see **CLINICAL STUDIES** – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). Hulio has not been studied in patients aged less than 2 years. **_Enthesitis-Related Arthritis_** Hulio is indicated for the treatment of active enthesitis-related arthritis in patients, 6 years of age and older, who have had an inadequate response to, or who are intolerant of, conventional therapy. **Pediatric Crohn's Disease** Hulio is indicated for reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients, 6 years of age and older, with moderately to severely active Crohn’s disease who have had an inadequate response to conventional therapy. **Pediatric Plaque Psoriasis** Hulio is indicated for the treatment of severe chronic plaque psoriasis in children and adolescents from 4 years of age who have had an inadequate response to or are inappropriate candidates for topical therapy and phototherapy. **Adolescent Hidradenitis Suppurativa** Hulio is indicated for the treatment of active moderate to severe hidradenitis suppurativa (acne inversa) in adolescents from 12 years of age with an inadequate response to conventional systemic hidradenitis suppurativa (HS) therapy. **Pediatric Uveitis** Hulio is indicated for the treatment of chronic non-infectious anterior uveitis in pediatric patients 2 years of age and older who have had an inadequate response to or are intolerant to conventional therapy, or in whom conventional therapy is inappropriate.
**Contraindications** Hypersensitivity to the active substance or to any of the excipients listed in section “List of excipients” – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_. Active tuberculosis or other severe infections such as sepsis, abscesses, and opportunistic infections. Moderate to severe heart failure (NYHA class III/IV).
L04AB04
adalimumab
Manufacturer Information
ZUELLIG PHARMA PTE. LTD.
Terumo Yamaguchi D&D Corporation (Drug Product Manufacturer & Primary Packager)
Active Ingredients
Documents
Package Inserts
Hulio Pre-filled Syringe Package Insert.pdf
Approved: November 2, 2021
