DEMEROL
These highlights do not include all the information needed to use DEMEROL™ INJECTION safely and effectively. See full prescribing information for DEMEROL INJECTION. DEMEROL™ (meperidine hydrochloride injection), for subcutaneous, intramuscular, and intravenous use, CII Initial U.S. Approval: 1942
b31d1308-28c3-43f4-e0a6-2f3ed76b8975
HUMAN PRESCRIPTION DRUG LABEL
Apr 5, 2024
Hospira, Inc.
DUNS: 141588017
Products 7
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
MEPERIDINE HYDROCHLORIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 50 mg/mL Syringe Cello Pack
NDC 0409-1418-01
Demerol™
CII
meperidine hydrochloride
injection, USP
50 mg / mL
For Intramuscular, Subcutaneous, or Intravenous Use
10 NexJect™ 1 mL Single-dose syringes with luer lock
Rx only
Needle not included
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between
15°C to 30°C (59°F to 86°F). [See USP Controlled Room Temperature.]
Sterile Aqueous Injection
Each mL contains 50 mg meperidine hydrochloride (equivalent to 43.58 mg
meperidine), NaOH and HCl for pH adjustment, in water for injection.
For usual dosage and route of administration, see package insert.
Demerol™ is a registered trademark of Sanofi Pharmaceuticals, Inc.
PAA189961
Distributed by Hospira, Inc.
Lake Forest, IL 60045 USA
Hospira

Boxed Warning section
WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF DEMEROL INJECTION
See full prescribing information for complete boxed warning.
•
**DEMEROL Injection exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and reassess regularly for these behaviors and conditions. (****5.1****)**
•
**Serious, life-threatening, or fatal respiratory depression may occur with use of DEMEROL Injection, especially during initiation or following a dosage increase. To reduce the risk of respiratory depression, proper dosing and titration of DEMEROL Injection are essential. (****5.2****)**
•
**Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate. (****5.3****,****7****)**
•
**If opioid use is required for an extended period of time in a pregnant woman, advise the patient of the risk of Neonatal Opioid Withdrawal Syndrome, which may be life-threatening if not recognized and treated. Ensure that management by neonatology experts will be available at delivery. (****5.4****)**
•
**Concomitant use with CYP3A4 inhibitors (or discontinuation of CYP3A4 inducers) can result in a fatal overdose of meperidine. (****5.5****,****7****)**
•
**Concomitant use of DEMEROL Injection with Monoamine oxidase (MAO) inhibitors can result in coma, severe respiratory depression, cyanosis and hypotension. Use of DEMEROL Injection with MAO inhibitors is contraindicated. (****4****,****5.6****,****7****)**
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
DEMEROL Injection is contraindicated in patients with:
•
Significant respiratory depression [see Warnings and Precautions (5.2)]
•
Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.9)]
•
Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days [see Warnings and Precautions (5.6), Drug Interactions (7)]
•
Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.13)]
•
Hypersensitivity to meperidine (e.g., anaphylaxis) [see Adverse Reactions (6)]
•
Significant respiratory depression. (4)
•
Acute or severe bronchial asthma in an unmonitored setting or in absence of resuscitative equipment. (4)
•
Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days. (7)
•
Known or suspected gastrointestinal obstruction, including paralytic ileus. (4)
•
Hypersensitivity to meperidine or to any other ingredients of the product. (4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following serious adverse reactions are described, or described in greater detail, in other sections:
•
Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
•
Life-Threatening Respiratory Depression [see Warnings and Precautions (5.2)]
•
Interactions with Benzodiazepines or Other CNS Depressants [see Warnings and Precautions (5.3)]
•
Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.4)]
•
Opioid-Induced Hyperalgesia and Allodynia [see Warnings and Precautions (5.7)]
•
Serotonin Syndrome with Concomitant Use of Serotonergic Drugs [see Warnings and Precautions (5.8)]
•
Adrenal Insufficiency [see Warnings and Precautions (5.10)]
•
Severe Hypotension [see Warnings and Precautions (5.11)]
•
Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.13)]
•
Seizures [see Warnings and Precautions (5.14)]
•
Withdrawal [see Warnings and Precautions (5.15)]
The following adverse reactions associated with the use of meperidine were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The major hazards of meperidine, as with other opioid analgesics, are respiratory depression and, to a lesser degree, circulatory depression; respiratory arrest, shock, and cardiac arrest have occurred.
The most frequently observed adverse reactions include lightheadedness, dizziness, sedation, nausea, vomiting, and sweating. These effects seem to be more prominent in ambulatory patients and in those who are not experiencing severe pain. In such individuals, lower doses are advisable. Some adverse reactions in ambulatory patients may be alleviated if the patient lies down.
Other adverse reactions include:
Nervous System: Mood changes (e.g., euphoria, dysphoria), weakness, headache, agitation, tremor, involuntary muscle movements (e.g., muscle twitches, myoclonus), severe convulsions, transient hallucinations and disorientation, confusion, delirium, visual disturbances.
Inadvertent injection about a nerve trunk may result in sensory-motor paralysis which is usually, though not always, transitory.
Gastrointestinal: Dry mouth, constipation, biliary tract spasm.
Cardiovascular: Flushing of the face, tachycardia, bradycardia, palpitation,
hypotension [see Warnings and Precautions (5.18)], syncope, phlebitis
following intravenous injection.
Genitourinary: Urinary retention.
Allergic: Pruritus, urticaria, other skin rashes, wheal and flare over the
vein with intravenous injection.
Hypersensitivity reactions, anaphylaxis.
Histamine release leading to hypotension and/or tachycardia, flushing,
sweating, and pruritus.
Other: Pain at injection site; local tissue irritation and induration
following subcutaneous injection, particularly when repeated; antidiuretic
effect.
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-
threatening condition, have been reported during concomitant use of opioids
with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with
opioid use, more often following greater than one month of use.
Androgen deficiency: Cases of androgen deficiency have occurred with use of
opioids for an extended period of time [see Clinical Pharmacology (12.2)].
Hyperalgesia and Allodynia: Cases of hyperalgesia and allodynia have been
reported with opioid therapy of any duration [see Warnings and Precautions (5.7)].
Hypoglycemia: Cases of hypoglycemia have been reported in patients taking
opioids. Most reports were in patients with at least one predisposing risk
factor (e.g., diabetes).
Most common adverse reactions were lightheadedness, dizziness, sedation, nausea, vomiting and sweating. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Hospira, Inc. at 1-800-441-4100, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Table 1 includes clinically significant drug interactions with DEMEROL Injection.
Table 1: Clinically Significant Drug Interactions with DEMEROL Injection|
Monoamine Oxidase Inhibitors (MAOIs) | |
|
Clinical Impact: |
Meperidine is contraindicated in patients who are receiving monoamine oxidase (MAO) inhibitors or those who have recently received such agents. Therapeutic doses of meperidine have occasionally precipitated unpredictable, severe, and occasionally fatal reactions in patients who have received such agents within 14 days. The mechanism of these reactions is unclear but may be related to a preexisting hyperphenylalaninemia. Some have been characterized by coma, severe respiratory depression, cyanosis, and hypotension, and have resembled the syndrome of acute narcotic overdose. Serotonin syndrome with agitation, hyperthermia, diarrhea, tachycardia, sweating, tremors, and impaired consciousness may also occur. In other reactions the predominant manifestations have been hyperexcitability, convulsions, tachycardia, hyperpyrexia, and hypertension [see Warnings and Precautions (5.6)]. |
|
Intervention: |
Do not use DEMEROL Injection in patients taking MAOIs or within 14 days of stopping such treatment. Intravenous hydrocortisone or prednisolone have been used to treat severe reactions, with the addition of intravenous chlorpromazine in those cases exhibiting hypertension and hyperpyrexia. The usefulness and safety of narcotic antagonists in the treatment of these reactions is unknown. |
|
Examples: |
Phenelzine, tranylcypromine, linezolid |
|
Inhibitors of CYP3A4 and CYP2B6 | |
|
Clinical Impact: |
The concomitant use of DEMEROL Injection and CYP3A4 or CYP2B6 inhibitors can increase the plasma concentration of meperidine, resulting in increased or prolonged opioid effects. These effects could be more pronounced with concomitant use of DEMEROL Injection and CYP2B6 and CYP3A4 inhibitors, particularly when an inhibitor is added after a stable dose of DEMEROL Injection is achieved [see Warnings and Precautions (5.5)]. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the meperidine plasma concentration will decrease [see Clinical Pharmacology (12.3)], potentially resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to meperidine. |
|
Intervention: |
If concomitant use is necessary, consider dosage reduction of DEMEROL Injection until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals. If a CYP3A4 or CYP2B6 inhibitor is discontinued, consider increasing the DEMEROL Injection dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. |
|
Examples: |
Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconizole), protease inhibitors (e.g., ritonavir) |
|
CYP3A4 and CYP2B6 Inducers | |
|
Clinical Impact: |
The concomitant use of DEMEROL Injection and CYP3A4 inducers or CYP2B6 inducers can decrease the plasma concentration of meperidine [see Clinical Pharmacology (12.3)], resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to meperidine [see Warnings and Precautions (5.5)]. After stopping a CYP3A4 or CYP2B6 inducer, as the effects of the inducer decline, the meperidine plasma concentration will increase [see Clinical Pharmacology (12.3)], which could increase or prolong both the therapeutic effects and adverse reactions and may cause serious respiratory depression. |
|
Intervention: |
If concomitant use is necessary, consider increasing the DEMEROL Injection dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. If a CYP3A4 or CYP2B6 inducer is discontinued, consider DEMEROL Injection dosage reduction and monitor for signs of respiratory depression. |
|
Examples: |
Rifampin, carbamazepine, phenytoin |
|
Benzodiazepines and Other Central Nervous System (CNS) Depressants | |
|
Clinical Impact: |
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension respiratory depression, profound sedation, coma, and death [see Warnings and Precautions (5.3)]. |
|
Intervention: |
Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Monitor patients closely for signs of respiratory depression and sedation. |
|
Examples: |
Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol. |
|
Serotonergic Drugs | |
|
Clinical Impact: |
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome [see Warnings and Precautions (5.8)]. |
|
Intervention: |
If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue DEMEROL Injection if serotonin syndrome is suspected. |
|
Examples: |
Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). |
|
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics | |
|
Clinical Impact: |
May reduce the analgesic effect of DEMEROL Injection and/or precipitate withdrawal symptoms. |
|
Intervention: |
Avoid concomitant use. |
|
Examples: |
Butorphanol, nalbuphine, pentazocine, buprenorphine. |
|
Muscle Relaxants | |
|
Clinical Impact: |
Meperidine may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. |
|
Intervention: |
Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of DEMEROL Injection and/or the muscle relaxant as necessary. |
|
Diuretics | |
|
Clinical Impact: |
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. |
|
Intervention: |
Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. |
|
Anticholinergic Drugs | |
|
Clinical Impact: |
The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. |
|
Intervention: |
Monitor patients for signs of urinary retention or reduced gastric motility when DEMEROL Injection is used concomitantly with anticholinergic drugs. |
|
Acyclovir | |
|
Clinical Impact: |
The concomitant use of acyclovir may increase the plasma concentrations of meperidine and its metabolite, normeperidine. |
|
Intervention: |
If concomitant use of acyclovir and DEMEROL Injection is necessary, monitor patients for respiratory depression and sedation at frequent intervals. |
|
Cimetidine | |
|
Clinical Impact: |
The concomitant use of cimetidine may reduce the clearance and volume of distribution of meperidine also the formation of the metabolite, normeperidine, in healthy subjects |
|
Intervention: |
If concomitant use cimetidine and DEMEROL Injection is necessary, monitor patients for respiratory depression and sedation at frequent intervals. |
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics: Avoid use with DEMEROL Injection because they may reduce analgesic effect of DEMEROL Injection or precipitate withdrawal symptoms. (7)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
DEMEROL Injection is a clear, colorless, sterile aqueous solution, available in the following dosage forms and strengths:
•
Single-dose Carpuject™ cartridge with Luer Lock for the Carpuject Syringe System, ONLY to be used with Carpuject™ Holder, and available in the following strengths: 25 mg/mL, 50 mg/mL, 75 mg/mL, and 100 mg/mL.
•
Multiple-dose vials containing 0.1% metacresol as a preservative, available in the following strength: 1,500 mg/30 mL (50 mg/mL).
•
Single-dose NexJectTM Prefilled Syringe with Luer Lock, available in the following strengths: 25 mg/mL and 50 mg/mL.
•
Injectable, Carpuject™ Single-Dose cartridge with Luer Lock for the Carpuject Syringe System, to be used ONLY with Carpuject™ Holder: 25 mg/mL, 50 mg/mL, 75 mg/mL, and 100 mg/mL. (3)
•
Injectable, Multiple-dose vials: 1,500 mg/30 mL (50 mg/mL). (3)
•
Injectable, NexJect™ Single-dose Prefilled Syringe with Luer Lock: 25 mg/mL and 50 mg/mL. (3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Use of opioid analgesics for an extended period of time during pregnancy may cause neonatal opioid withdrawal syndrome [see Warnings and Precautions (5.4)]. Available data with DEMEROL Injection are insufficient to inform a drug-associated risk for major birth defects and miscarriage or adverse maternal outcomes. There are adverse outcomes reported with fetal exposure to opioid analgesics (see Clinical Considerations). Formal animal reproduction studies have not been conducted with meperidine. Neural tube defects (exencephaly and cranioschisis) have been reported in hamsters administered a single bolus dose of meperidine during a critical period of organogenesis at 0.85 and 1.5 times the total human daily dose of 1200 mg [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Use of opioid analgesics for an extended period of time during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn. Observe newborns for symptoms of neonatal opioid withdrawal syndrome and manage accordingly [see Warnings and Precautions (5.4)].
Labor or Delivery
Opioids cross the placenta and may produce respiratory depression and psycho- physiologic effects in neonates. An opioid antagonist, such as naloxone, must be available for reversal of opioid-induced respiratory depression in the neonate. DEMEROL Injection is not recommended for use in pregnant women during or immediately prior to labor, when other analgesic techniques are more appropriate. Opioid analgesics, including DEMEROL Injection, can prolong labor through actions which temporarily reduce the strength, duration, and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilation, which tends to shorten labor. Monitor neonates exposed to opioid analgesics during labor for signs of excess sedation and respiratory depression.
Data
Animal Data
Formal reproductive and developmental toxicology studies for meperidine have not been completed.
In a published study, neural tube defects (exencephaly and cranioschisis) were noted following subcutaneous administration of meperidine hydrochloride (127 and 218 mg/kg, respectively) on Gestation Day 8 to pregnant hamsters (0.85 and 1.5 times the total daily dose of 1200 mg/day based on body surface area). The findings cannot be clearly attributed to maternal toxicity.
8.2 Lactation
Risk Summary
Meperidine appears in the milk of nursing mothers receiving the drug. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for DEMEROL Injection and any potential adverse effects on the breastfed infant from DEMEROL Injection or from the underlying maternal condition.
Clinical Considerations
Monitor infants exposed to DEMEROL Injection through breast milk for excess sedation and respiratory depression. Withdrawal symptoms can occur in breastfed infants when maternal administration of an opioid analgesic is stopped, or when breastfeeding is stopped.
8.3 Females and Males of Reproductive Potential
Infertility
Use of opioids for an extended period of time may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Adverse Reactions (6), Clinical Pharmacology (12.2), Nonclinical Pharmacology (13.1)].
8.4 Pediatric Use
The safety and efficacy of DEMEROL Injection in patients less than 18 years of age have not been established.
The safety and effectiveness of meperidine in pediatric patients has not been established. Literature reports indicate that meperidine has a slower elimination rate in neonates and young infants compared to older children and adults. Neonates and young infants may also be more susceptible to the effects, especially the respiratory depressant effects. If meperidine use is contemplated in neonates or young infants, any potential benefits of the drug need to be weighed against the relative risk of the patient.
8.5 Geriatric Use
Elderly patients (aged 65 years or older) may have increased sensitivity to meperidine. In general, use caution when selecting a dosage for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of DEMEROL Injection slowly in geriatric patients and monitor closely for signs of central nervous system and respiratory depression [see Warnings and Precautions (5.2)].
Meperidine is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Hepatic Impairment
Accumulation of meperidine and/or its active metabolite, normeperidine, can also occur in patients with hepatic impairment. Elevated serum levels have been reported to cause central nervous system excitatory effects. Meperidine should therefore be used with caution in patients with hepatic impairment. Titrate the dosage of DEMEROL Injection slowly in patients with hepatic impairment and monitor closely for signs of central nervous system and respiratory depression.
8.7 Renal Impairment
Accumulation of meperidine and/or its active metabolite, normeperidine, can occur in patients with renal impairment. Meperidine should therefore be used with caution in patients with renal impairment. Titrate the dosage of DEMEROL Injection slowly in patients with renal impairment and monitor closely for signs of central nervous system and respiratory depression.
•
Pregnancy: May cause fetal harm. (8.1)
•
Geriatric Patients: Use caution during dose selection, starting at the low end of the dosing range while carefully monitoring for side effects. (8.5)
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
DEMEROL Injection contains meperidine, a Schedule II controlled substance.
9.2 Abuse
DEMEROL Injection contains meperidine, a substance with high potential for misuse and abuse, which can lead to the development of substance use disorder, including addiction [see Warnings and Precautions (5.1)].
Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a healthcare provider or for whom it was not prescribed.
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence.
Misuse and abuse of DEMEROL Injection increases risk of overdose, which may lead to central nervous system and respiratory depression, hypotension, seizures, and death. The risk is increased with concurrent abuse of DEMEROL Injection with alcohol and/or other CNS depressants. Abuse of and addiction to opioids in some individuals may not be accompanied by concurrent tolerance and symptoms of physical dependence. In addition, abuse of opioids can occur in the absence of addiction.
All patients treated with opioids require careful and frequent reevaluation for signs of misuse, abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use. Patients at high risk of DEMEROL Injection abuse include those with a history of prolonged use of any opioid, including products containing meperidine, those with a history of drug or alcohol abuse, or those who use DEMEROL Injection in combination with other abused drugs.
“Drug-seeking” behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated “loss” of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). “Doctor shopping” (visiting multiple prescribers to obtain additional prescriptions) is common among people who abuse drugs and people with substance use disorder. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with inadequate pain control.
DEMEROL Injection, like other opioids, can be diverted for nonmedical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of DEMEROL Injection
Abuse of DEMEROL Injection poses a risk of overdose and death. The risk is increased with concurrent abuse of DEMEROL Injection with alcohol and/or other CNS depressants.
Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
9.3 Dependence
Both tolerance and physical dependence can develop during use of opioid therapy.
Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose).
Physical dependence is a state that develops as a result of a physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug.
Withdrawal may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued use.
DEMEROL Injection should not be abruptly discontinued in a physically- dependent patient [see Dosage and Administration (2.4)]. If DEMEROL Injection is abruptly discontinued in a physically-dependent patient, a withdrawal syndrome may occur, typically characterized by restlessness, lacrimation, rhinorrhea, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically-dependent on opioids will also be physically-dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations (8.1)].
DESCRIPTION SECTION
11 DESCRIPTION
DEMEROL (meperidine hydrochloride injection) is an opioid agonist available as a sterile aqueous solution, for intramuscular, intravenous, or subcutaneous administration. It contains meperidine hydrochloride as the active pharmaceutical ingredient. Meperidine hydrochloride chemical name is 4‑Piperidinecarboxylic acid, 1‑methyl-4-phenyl-,ethyl ester, hydrochloride. The molecular weight is 283.79 g/mol. Its molecular formula is C15H21NO2·HCl, and it has the following chemical structure.

Meperidine hydrochloride is a white crystalline substance with a melting point of 186° C to 189° C, and it is readily soluble in water.
DEMEROL (meperidine hydrochloride injection) is available as:
Single-dose Carpuject cartridge with Luer Lock for the Carpuject Syringe System: 25 mg/mL, 50 mg/mL, 75 mg/mL, and 100 mg/mL. Each mL of Single-dose cartridge contains 25 mg, 50 mg, 75 mg or 100 mg of meperidine hydrochloride USP (equivalent to 21.79 mg, 43.58 mg, 65.36 mg or 87.15 mg of meperidine), respectively, and sodium hydroxide NF, and hydrochloric acid NF as pH adjusters, in water for injection. Only the 25 mg strength contains 3.8 mg of sodium chloride USP as isotonicity agent.
Multiple-dose vials: 1,500 mg/30 mL (50 mg/mL) strength. Each mL of vial contains 50 mg of meperidine hydrochloride USP (equivalent to 43.58 mg of meperidine), 1 mg of meta-cresol USP, as a preservative, and sodium hydroxide NF, and hydrochloric acid NF as pH adjusters, in water for injection.
Single-dose NexJect™ Prefilled Syringe with Luer Lock: 25 mg/mL and 50 mg/mL strengths. Each mL contains 25 mg or 50 mg of meperidine hydrochloride USP (equivalent to 21.79 mg or 43.58 mg of meperidine), respectively, and sodium hydroxide NF, and hydrochloric acid NF as pH adjusters, in water for injection. Only the 25 mg strength contains 3.8 mg of sodium chloride USP as isotonicity agent.
The pH of DEMEROL (meperidine hydrochloride injection) solutions is between 3.5 and 6.0.
DEMEROL (meperidine hydrochloride injection) 5 percent solution has a specific gravity of 1.0086 at 20°C, and the 10 percent solution has a specific gravity of 1.0165 at 20°C.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Meperidine hydrochloride is an opioid agonist with multiple actions qualitatively similar to those of morphine; the most prominent of these involve the central nervous system and organs composed of smooth muscle. The principal actions of therapeutic value are analgesia and sedation.
12.2 Pharmacodynamics
Effects on the Central Nervous System
Meperidine produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Meperidine causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Meperidine causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm, resulting in constipation. Other opioid- induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects of the Cardiovascular System
Meperidine produces peripheral vasodilation which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, and sweating and/or orthostatic hypotension.
Effects on the Endocrine System
Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormones (LH) in humans [see Adverse Reactions (6)]. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Use of opioids for an extended period of time may influence the hypothalamic- pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date [see Adverse Reactions (6)].
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships
The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with opioid agonists. The minimum effective analgesic concentration of meperidine for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome and/or the development of analgesic tolerance [see Dosage and Administration (2.1, 2.2)].
Meperidine, in 60 mg to 80 mg parenteral doses, is approximately equivalent in analgesic effect to 10 mg of morphine. The onset of action is slightly more rapid than with morphine, and the duration of action is slightly shorter. Meperidine is significantly less effective by the oral than by the parenteral route, but the exact ratio of oral to parenteral effectiveness is unknown.
Concentration–Adverse Reaction Relationships
There is a relationship between increasing meperidine plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions [see Dosage and Administration (2.1, 2.2)].
12.3 Pharmacokinetics
Elimination
The half-life of meperidine is 2 to 5 hours, and the half-life of normeperidine is 15 to 30 hours.
Metabolism
Meperidine is metabolized through biotransformation. In vitro data show meperidine is metabolized to normeperidine in liver mainly by CYP3A4 and CYP2B6.
Excretion
Meperidine and normeperidine are excreted by kidneys.
Specific Population
Hepatic Impairment
The elimination half-life is 3 to 8 hours in healthy volunteers and is 1.3 to 2 times greater in post‑operative or cirrhotic patients.
Age
In clinical studies reported in the literature, changes in several pharmacokinetic parameters with increasing age have been observed. The initial volume of distribution and steady-state volume of distribution may be higher in elderly patients than in younger patients. The free fraction of meperidine in plasma may be higher in patients over 45 years of age than in younger patients.
Drug Interactions Studies
Phenytoin: The hepatic metabolism of meperidine may be enhanced by phenytoin. Concomitant administration resulted in reduced half-life and bioavailability with increased clearance of meperidine in healthy subjects; however, blood concentrations of normeperidine were increased [see Drug Interactions (7)].
Ritonavir: Plasma concentrations of the active metabolite normeperidine may be increased by ritonavir [see Drug Interactions (7)].
Acyclovir: Plasma concentrations of meperidine and its metabolite, normeperidine, may be increased by acyclovir [see Drug Interactions (7)].
Cimetidine: Cimetidine reduced the clearance and volume of distribution of meperidine and also the formation of the metabolite, normeperidine, in healthy subjects [see Drug Interactions (7)].
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate the carcinogenic potential of meperidine have not been conducted.
Mutagenesis
Studies in animals to evaluate the mutagenic potential of meperidine have not been conducted.
Impairment of Fertility
Studies to determine the effect of meperidine on fertility have not been conducted.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Addiction, Abuse, and Misuse
Inform patients that the use of DEMEROL Injection, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose and death [see Warnings and Precautions (5.1)]. Instruct patients not to share DEMEROL Injection with others and to take steps to protect DEMEROL Injection from theft or misuse.
Life-Threatening Respiratory Depression
Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when DEMEROL Injection or when the dosage is increased, and that it can occur even at recommended dosages [see Warnings and Precautions (5.2)].
Hyperalgesia and Allodynia
Advise patients to inform their healthcare provider if they experience symptoms of hyperalgesia, including worsening pain, increased sensitivity to pain, or new pain [see Warnings and Precautions (5.7), Adverse Reactions (6)].
Serotonin Syndrome
Inform patients that opioids could cause a rare but potentially life- threatening condition called serotonin syndrome resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop after discharge from the hospital. Instruct patients to inform their healthcare provider if they are taking, or plan to take serotonergic medications [see Warnings and Precautions (5.8), Drug Interactions (7)].
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention [see Adverse Reactions (6), Clinical Pharmacology (12.1)].
SPL UNCLASSIFIED SECTION
Distributed by Hospira, Inc., Lake Forest, IL 60045 USA
For Medical Information about DEMEROL Injection, please visit www.pfizermedinfo.com or call 1‑800‑438‑1985.

LAB-0846-10.0
INSTRUCTIONS FOR USE SECTION
INSTRUCTIONS FOR USE
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if color is darker than pale yellow, if it is discolored in any other way, or if it contains a precipitate.
Instructions for use - Carpuject™ Single-dose Cartridge
Carpuject™ Single-dose cartridges with Luer Lock are packaged in a Slim-Pak™ tamper detection package. Note that a needle is not included.
Before use, read all instructions for using the Carpuject™ Syringe, which are contained in the product insert for the reusable Carpuject™ Holder before use.
Carpuject™ Single-dose cartridges are to be used ONLY with Carpuject™ Holders.
NOTE: To prevent needlestick injuries, do not recap, purposely bend, or break by hand used needles. Do not recap, purposely bend, or break by hand blunt Cannulas.
Instructions for use - NexJect™ Single-dose Prefilled Syringe
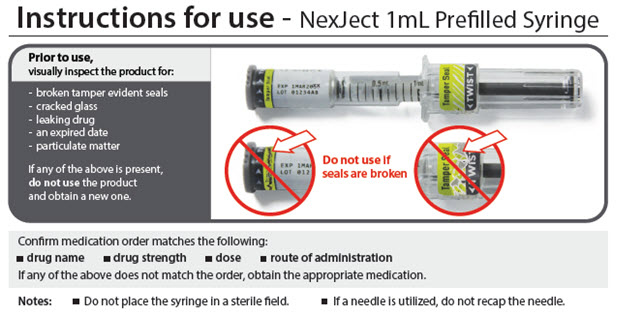
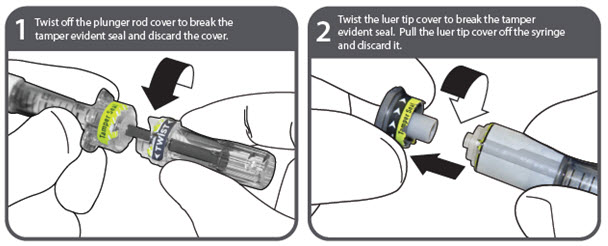

NOTE: To prevent needlestick injuries, do not recap, purposely bend, or break by hand used needles. Do not recap, purposely bend, or break by hand blunt Cannulas.
Distributed by Hospira, Inc., Lake Forest, IL 60045 USA

LAB-1387-2.0
Revised: 12/2023
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Boxed Warning |
12/2023 |
|
Indications and Usage (1) |
12/2023 |
|
Dosage and Administration (2.1, 2.2) |
12/2023 |
|
Warnings and Precautions (5.7) |
12/2023 |
OVERDOSAGE SECTION
10 OVERDOSAGE
Clinical Presentation
Acute overdose with meperidine can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, hypoglycemia, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology (12.2)]. In severe overdose, particularly by the intravenous route, apnea, circulatory collapse, cardiac arrest, and death may occur.
Accumulation of normeperidine as in chronic use or possibly following introduction of a concomitant CYP3A4 inducer presents as excitatory syndrome including hallucinations, tremors, muscle twitches, dilated pupils, hyperactive reflexes, and convulsions.
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support measures.
Opioid antagonists, such as naloxone, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to meperidine overdose, administer an opioid antagonist.
Because the duration of opioid reversal is expected to be less than the duration of action of meperidine in DEMEROL Injection, carefully monitor the patient until spontaneous respiration is reliably re-established. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product's prescribing information.
In an individual physically dependent on opioids, administration of the recommended usual dosage of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically-dependent patient, administration of the antagonist should be begun with care and by titration with smaller than usual doses of the antagonist.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
For Parenteral Use
DEMEROL (meperidine hydrochloride injection) is clear and colorless.
DEMEROL (meperidine hydrochloride injection) is supplied as a sterile solution in a multiple-dose vial, single-dose Carpuject™ cartridges for use ONLY with the Carpuject™ Holders and NexJect™ prefilled syringes for subcutaneous, intramuscular, and intravenous administration, and available as follows:
|
Unit of Sale |
Concentration |
|---|---|
|
NDC 0409-1181-30 |
1,500 mg/30 mL |
|
NDC 0409-1176-30 |
25 mg/mL |
|
NDC 0409-1178-30 |
50 mg/mL |
|
NDC 0409-1179-30 |
75 mg/mL |
|
NDC 0409-1180-69 |
100 mg/mL |
|
NDC 0409-1362-01 |
25 mg/mL |
|
NDC 0409-1418-01 |
50 mg/mL |
Carpuject™ Single-dose cartridges are packaged in a Slim-Pak tamper detection package.
Note that a needle is not included with Carpuject™ Single-dose cartridges and Nexject™ Single-dose Prefilled Syringes.
Carpuject and NexJectTM Single-dose products: Discard unused portion.
Multiple-dose vials: Discard unused portion after 28 days.
Store at 20°C to 25°C (68°F to 77°F), excursions permitted between 15°C to 30°C (59°F to 86°F). [See USP Controlled Room Temperature.]
