Valproate Sodium
These highlights do not include all the information needed to use VALPROATE SODIUM INJECTION safely and effectively. See full prescribing information for VALPROATE SODIUM INJECTION. VALPROATE SODIUM injection for intravenous injection Initial U.S. Approval: 1996
856ecdad-a8e0-4bda-a217-cd7948ddfa59
HUMAN PRESCRIPTION DRUG LABEL
Mar 5, 2024
Athenex Pharmaceutical Division, LLC.
DUNS: 080318964
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
valproate sodium
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
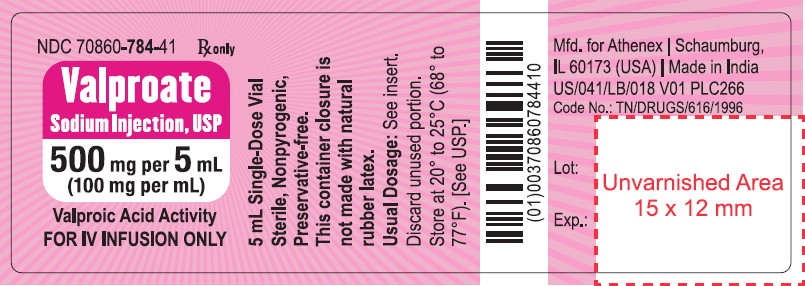
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC 70860-784-41
Valproate Sodium Injection, USP
500 mg per 5 mL (100 mg per mL)
Valproic Acid Activity
For IV Infusion Only
5 mL Single-Dose Vial
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Epilepsy
Valproate Sodium Injection is indicated as an intravenous alternative in patients for whom oral administration of valproate products is temporarily not feasible in the following conditions:
Valproate Sodium Injection is indicated as monotherapy and adjunctive therapy in the treatment of patients with complex partial seizures that occur either in isolation or in association with other types of seizures. Valproate Sodium Injection is also indicated for use as sole and adjunctive therapy in the treatment of patients with simple and complex absence seizures, and adjunctively in patients with multiple seizure types that include absence seizures.
Simple absence is defined as very brief clouding of the sensorium or loss of consciousness accompanied by certain generalized epileptic discharges without other detectable clinical signs. Complex absence is the term used when other signs are also present.
See Warnings and Precautions ( 5.1) for statement regarding fatal hepatic dysfunction.
1.2 Important Limitations
Because of the risk to the fetus of decreased IQ, neurodevelopmental disorders, neural tube defects, and other major congenital malformations, which may occur very early in pregnancy, valproate should not be used to treat women with epilepsy or bipolar disorder who are pregnant or who plan to become pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. Valproate should not be administered to a woman of childbearing potential unless other medications have failed to provide adequate symptom control or are otherwise unacceptable [see Warnings and Precautions ( 5.2, 5.3, 5.4) , Use in Specific Populations ( 8.1) , and Patient Counseling Information ( 17)] .
For prophylaxis of migraine headaches, valproate is contraindicated in women who are pregnant and in women of childbearing potential who are not using effective contraception [see Contraindications ( 4)] .
Valproate Sodium Injection is indicated as an intravenous alternative in patients in whom oral administration of valproate products is temporarily not feasible in the following conditions:
- Monotherapy and adjunctive therapy of complex partial seizures and simple and complex absence seizures; adjunctive therapy in patients with multiple seizure types that include absence seizures ( 1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
- Valproate Sodium Injection should not be administered to patients with hepatic disease or significant hepatic dysfunction [see Warnings and Precautions ( 5.1)] .
- Valproate Sodium Injection is contraindicated in patients known to have mitochondrial disorders caused by mutations in mitochondrial DNA polymerase γ (POLG; e.g., Alpers-Huttenlocher Syndrome) and children under two years of age who are suspected of having a POLG-related disorder [see Warnings and Precautions ( 5.1)] .
- Valproate Sodium Injection is contraindicated in patients with known hypersensitivity to the drug [see Warnings and Precautions ( 5.11)] .
- Valproate Sodium Injection is contraindicated in patients with known urea cycle disorders [see Warnings and Precautions ( 5.6)] .
- For use in prophylaxis of migraine headaches: Valproate is contraindicated in women who are pregnant and in women of childbearing potential who are not using effective contraception [see Warnings and Precautions ( 5.2, 5.3, 5.4) and Use in Specific Populations ( 8.1)].
- Hepatic disease or significant hepatic dysfunction ( 4, 5.1)
- Known mitochondrial disorders caused by mutations in mitochondrial DNA polymerase γ (POLG) ( 4, 5.1)
- Suspected POLG-related disorder in children under two years of age ( 4, 5.1)
- Known hypersensitivity to the drug ( 4, 5.11)
- Urea cycle disorders ( 4, 5.6)
- Prophylaxis of migraine headaches: Pregnant women, women of childbearing potential not using effective contraception ( 4, 8.1)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Epilepsy
Valproate Sodium Injection is for intravenous use only.
Use of Valproate Sodium Injection for periods of more than 14 days has not been studied. Patients should be switched to oral valproate products as soon as it is clinically feasible.
Valproate Sodium Injection should be administered as a 60 minute infusion (but not more than 20 mg/min) with the same frequency as the oral products, although plasma concentration monitoring and dosage adjustments may be necessary.
In one clinical safety study, approximately 90 patients with epilepsy and with no measurable plasma levels of valproate were given single infusions of Valproate Sodium Injection (up to 15 mg/kg and mean dose of 1184 mg) over 5 to 10 minutes (1.5 to 3 mg/kg/min). Patients generally tolerated the more rapid infusions well [see Adverse Reactions ( 6.1)] . This study was not designed to assess the effectiveness of these regimens. For pharmacokinetics with rapid infusions, see Clinical Pharmacology ( 12.3) .
Initial Exposure to Valproate
The following dosage recommendations were obtained from studies utilizing oral divalproex sodium products.
Complex Partial Seizures
For adults and children 10 years of age or older.
Monotherapy (Initial Therapy)
Valproate Sodium Injection has not been systematically studied as initial therapy. Patients should initiate therapy at 10 to 15 mg/kg/day. The dosage should be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 mcg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made.
The probability of thrombocytopenia increases significantly at total trough valproate plasma concentrations above 110 mcg/mL in females and 135 mcg/mL in males. The benefit of improved seizure control with higher doses should be weighed against the possibility of a greater incidence of adverse reactions.
Conversion to Monotherapy
Patients should initiate therapy at 10 to 15 mg/kg/day. The dosage should be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 mcg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made. Concomitant antiepilepsy drug (AED) dosage can ordinarily be reduced by approximately 25% every 2 weeks. This reduction may be started at initiation of Valproate Sodium Injection therapy, or delayed by 1 to 2 weeks if there is a concern that seizures are likely to occur with a reduction. The speed and duration of withdrawal of the concomitant AED can be highly variable, and patients should be monitored closely during this period for increased seizure frequency.
Adjunctive Therapy
Valproate Sodium Injection may be added to the patient's regimen at a dosage of 10 to 15 mg/kg/day. The dosage may be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 mcg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made. If the total daily dose exceeds 250 mg, it should be given in divided doses.
In a study of adjunctive therapy for complex partial seizures in which patients were receiving either carbamazepine or phenytoin in addition to valproate, no adjustment of carbamazepine or phenytoin dosage was needed [see Clinical Studies ( 14)] . However, since valproate may interact with these or other concurrently administered AEDs as well as other drugs, periodic plasma concentration determinations of concomitant AEDs are recommended during the early course of therapy [see Drug Interactions ( 7)] .
Simple and Complex Absence Seizures
The recommended initial dose is 15 mg/kg/day, increasing at one week intervals by 5 to 10 mg/kg/day until seizures are controlled or side effects preclude further increases. The maximum recommended dosage is 60 mg/kg/day. If the total daily dose exceeds 250 mg, it should be given in divided doses.
A good correlation has not been established between daily dose, serum concentrations, and therapeutic effect. However, therapeutic valproate serum concentration for most patients with absence seizures is considered to range from 50 to 100 mcg/mL. Some patients may be controlled with lower or higher serum concentrations [see Clinical Pharmacology ( 12.3)] .
As the Valproate Sodium Injection dosage is titrated upward, blood concentrations of phenobarbital and/or phenytoin may be affected [see Drug Interactions ( 7.2)] .
Antiepilepsy drugs should not be abruptly discontinued in patients in whom the drug is administered to prevent major seizures because of the strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life.
Replacement Therapy
When switching from oral valproate products, the total daily dose of Valproate Sodium Injection should be equivalent to the total daily dose of the oral valproate product [see Clinical Pharmacology ( 12)] , and should be administered as a 60 minute infusion (but not more than 20 mg/min) with the same frequency as the oral products, although plasma concentration monitoring and dosage adjustments may be necessary. Patients receiving doses near the maximum recommended daily dose of 60 mg/kg/day, particularly those not receiving enzyme-inducing drugs, should be monitored more closely. If the total daily dose exceeds 250 mg, it should be given in a divided regimen. There is no experience with more rapid infusions in patients receiving Valproate Sodium Injection as replacement therapy. However, the equivalence shown between Valproate Sodium Injection and oral valproate products (divalproex sodium) at steady state was only evaluated in an every 6 hour regimen. Whether, when Valproate Sodium Injection is given less frequently (i.e., twice or three times a day), trough levels fall below those that result from an oral dosage form given via the same regimen, is unknown. For this reason, when Valproate Sodium Injection is given twice or three times a day, close monitoring of trough plasma levels may be needed.
2.2 General Dosing Advice
Dosing in Elderly Patients
Due to a decrease in unbound clearance of valproate and possibly a greater sensitivity to somnolence in the elderly, the starting dose should be reduced in these patients. Dosage should be increased more slowly and with regular monitoring for fluid and nutritional intake, dehydration, somnolence, and other adverse reactions. Dose reductions or discontinuation of valproate should be considered in patients with decreased food or fluid intake and in patients with excessive somnolence. The ultimate therapeutic dose should be achieved on the basis of both tolerability and clinical response [see Warnings and Precautions ( 5.13), Use in Specific Populations ( 8.5) and Clinical Pharmacology ( 12.3)] .
Dose-Related Adverse Reactions
The frequency of adverse effects (particularly elevated liver enzymes and thrombocytopenia) may be dose-related. The probability of thrombocytopenia appears to increase significantly at total valproate concentrations of ≥ 110 mcg/mL (females) or ≥ 135 mcg/mL (males) [see Warnings and Precautions ( 5.7)] . The benefit of improved therapeutic effect with higher doses should be weighed against the possibility of a greater incidence of adverse reactions.
Administration
Rapid infusion of Valproate Sodium Injection has been associated with an increase in adverse reactions. There is limited experience with infusion times of less than 60 minutes or rates of infusion > 20 mg/min in patients with epilepsy [see Adverse Reactions ( 6)] .
Valproate Sodium Injection should be administered intravenously as a 60 minute infusion, as noted above. It should be diluted with at least 50 mL of a compatible diluent. Any unused portion of the vial contents should be discarded.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Compatibility and Stability
Valproate Sodium Injection was found to be physically compatible and chemically stable in the following parenteral solutions for at least 24 hours when stored in glass or polyvinyl chloride (PVC) bags at controlled room temperature 15° to 30°C (59° to 86°F).
- dextrose (5%) injection, USP
- sodium chloride (0.9%) injection, USP
- lactated ringer's injection, USP
2.3 Dosing in Patients Taking Rufinamide
Patients stabilized on rufinamide before being prescribed valproate should begin valproate therapy at a low dose, and titrate to a clinically effective dose [see Drug Interactions ( 7.2)] .
Valproate Sodium Injection is intended for intravenous use only.
- Epilepsy
- Complex Partial Seizures in Adults and Children 10 years of age or older: Initial dose is 10 to 15 mg/kg/day, increasing at 1 week intervals by 5 to 10 mg/kg/day to achieve optimal clinical response. Maximum recommended dose is 60 mg/kg/day ( 2.1)
- Simple and Complex Absence Seizures: Initial dose is 10 to 15 mg/kg/day, increasing at 1 week intervals by 5 to 10 mg/kg/day to achieve optimal clinical response. Maximum recommended dose is 60 mg/kg/day ( 2.1)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Valproate Sodium Injection, USP, equivalent to 100 mg of valproic acid per mL, is a clear, colorless solution in 5 mL single-dose vials, available in cartons of 10 vials.
Recommended storage: Store vials at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
No preservatives have been added. Unused portion of container should be discarded.
Injection: 100 mg per mL in a 5 mL single-dose vial ( 3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), including Valproate Sodium Injection, during pregnancy. Encourage women who are taking Valproate Sodium Injection during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling toll-free 1-888-233-2334 or visiting the website http://www.aedpregnancyregistry.org/. This must be done by the patient herself.
Risk Summary
For use in prophylaxis of migraine headaches, valproate is contraindicated in women who are pregnant and in women of childbearing potential who are not using effective contraception [see Contraindications ( 4)] .
For use in epilepsy or bipolar disorder, valproate should not be used to treat women who are pregnant or who plan to become pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable [see Boxed Warningand Warnings and Precautions ( 5.2, 5.3)] . Women with epilepsy who become pregnant while taking valproate should not discontinue valproate abruptly, as this can precipitate status epilepticus with resulting maternal and fetal hypoxia and threat to life.
Maternal valproate use during pregnancy for any indication increases the risk of congenital malformations, particularly neural tube defects including spina bifida, but also malformations involving other body systems (e.g., craniofacial defects including oral clefts, cardiovascular malformations, hypospadias, limb malformations). This risk is dose-dependent; however, a threshold dose below which no risk exists cannot be established. In uteroexposure to valproate may also result in hearing impairment or hearing loss. Valproate polytherapy with other AEDs has been associated with an increased frequency of congenital malformations compared with AED monotherapy. The risk of major structural abnormalities is greatest during the first trimester; however, other serious developmental effects can occur with valproate use throughout pregnancy. The rate of congenital malformations among babies born to epileptic mothers who used valproate during pregnancy has been shown to be about four times higher than the rate among babies born to epileptic mothers who used other anti-seizure monotherapies [see Warnings and Precautions ( 5.2) and Data (Human)] .
Epidemiological studies have indicated that children exposed to valproate in uterohave lower IQ scores and a higher risk of neurodevelopmental disorders compared to children exposed to either another AED in uteroor to no AEDs in utero [see Warnings and Precautions ( 5.3) and Data (Human)] .
An observational study has suggested that exposure to valproate products during pregnancy increases the risk of autism spectrum disorders [see Data (Human)] .
In animal studies, valproate administration during pregnancy resulted in fetal structural malformations similar to those seen in humans and neurobehavioral deficits in the offspring at clinically relevant doses [see Data (Animal)] .
There have been reports of hypoglycemia in neonates and fatal cases of hepatic failure in infants following maternal use of valproate during pregnancy.
Pregnant women taking valproate may develop hepatic failure or clotting abnormalities including thrombocytopenia, hypofibrinogenemia, and/or decrease in other coagulation factors, which may result in hemorrhagic complications in the neonate including death [see Warnings and Precautions ( 5.1, 5.8)].
Available prenatal diagnostic testing to detect neural tube and other defects should be offered to pregnant women using valproate.
Evidence suggests that folic acid supplementation prior to conception and during the first trimester of pregnancy decreases the risk for congenital neural tube defects in the general population. It is not known whether the risk of neural tube defects or decreased IQ in the offspring of women receiving valproate is reduced by folic acid supplementation. Dietary folic acid supplementation both prior to conception and during pregnancy should be routinely recommended for patients using valproate [see Warnings and Precautions ( 5.2, 5.4)] .
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
To prevent major seizures, women with epilepsy should not discontinue valproate abruptly, as this can precipitate status epilepticus with resulting maternal and fetal hypoxia and threat to life. Even minor seizures may pose some hazard to the developing embryo or fetus [see Warnings and Precautions ( 5.4)] . However, discontinuation of the drug may be considered prior to and during pregnancy in individual cases if the seizure disorder severity and frequency do not pose a serious threat to the patient.
Maternal adverse reactions
Pregnant women taking valproate may develop clotting abnormalities including thrombocytopenia, hypofibrinogenemia, and/or decrease in other coagulation factors, which may result in hemorrhagic complications in the neonate including death [see Warnings and Precautions ( 5.7)] . If valproate is used in pregnancy, the clotting parameters should be monitored carefully in the mother. If abnormal in the mother, then these parameters should also be monitored in the neonate.
Patients taking valproate may develop hepatic failure [see Boxed Warningand Warnings and Precautions ( 5.1)] . Fatal cases of hepatic failure in infants exposed to valproate in uterohave also been reported following maternal use of valproate during pregnancy.
Hypoglycemia has been reported in neonates whose mothers have taken valproate during pregnancy.
Data
Human
Neural tube defects and other structural abnormalities
There is an extensive body of evidence demonstrating that exposure to valproate in uteroincreases the risk of neural tube defects and other structural abnormalities. Based on published data from the CDC's National Birth Defects Prevention Network, the risk of spina bifida in the general population is about 0.06 to 0.07% (6 to 7 in 10,000 births) compared to the risk following in uterovalproate exposure estimated to be approximately 1 to 2% (100 to 200 in 10,000 births).
The NAAED Pregnancy Registry has reported a major malformation rate of 9 to 11% in the offspring of women exposed to an average of 1,000 mg/day of valproate monotherapy during pregnancy. These data show an up to a five-fold increased risk for any major malformation following valproate exposure in uterocompared to the risk following exposure in uteroto other AEDs taken as monotherapy. The major congenital malformations included cases of neural tube defects, cardiovascular malformations, craniofacial defects (e.g., oral clefts, craniosynostosis), hypospadias, limb malformations (e.g., clubfoot, polydactyly), and other malformations of varying severity involving other body systems [see Warnings and Precautions ( 5.2)] .
Effect on IQ and neurodevelopmental effects
Published epidemiological studies have indicated that children exposed to valproate in uterohave lower IQ scores than children exposed to either another AED in uteroor to no AEDs in utero. The largest of these studies is a prospective cohort study conducted in the United States and United Kingdom that found that children with prenatal exposure to valproate (n=62) had lower IQ scores at age 6 (97 [95% C.I. 94 to 101]) than children with prenatal exposure to the other anti-epileptic drug monotherapy treatments evaluated: lamotrigine (108 [95% C.I. 105 to 110]), carbamazepine (105 [95% C.I. 102 to 108]) and phenytoin (108 [95% C.I. 104 to 112]). It is not known when during pregnancy cognitive effects in valproate-exposed children occur. Because the women in this study were exposed to AEDs throughout pregnancy, whether the risk for decreased IQ was related to a particular time period during pregnancy could not be assessed [see Warnings and Precautions ( 5.3)] .
Although the available studies have methodological limitations, the weight of the evidence supports a causal association between valproate exposure in uteroand subsequent adverse effects on neurodevelopment, including increases in autism spectrum disorders and attention deficit/hyperactivity disorder (ADHD).
An observational study has suggested that exposure to valproate products during pregnancy increases the risk of autism spectrum disorders. In this study, children born to mothers who had used valproate products during pregnancy had 2.9 times the risk (95% confidence interval [CI]: 1.7 to 4.9) of developing autism spectrum disorders compared to children born to mothers not exposed to valproate products during pregnancy. The absolute risks for autism spectrum disorders were 4.4% (95% CI: 2.6% to 7.5%) in valproate-exposed children and 1.5% (95% CI: 1.5% to 1.6%) in children not exposed to valproate products. Another observational study found that children who were exposed to valproate in uterohad an increased risk of ADHD (adjusted HR 1.48; 95% CI, 1.09 to 2.00) compared with the unexposed children. Because these studies were observational in nature, conclusions regarding a causal association between in uterovalproate exposure and an increased risk of autism spectrum disorder and ADHD cannot be considered definitive.
Other
There are published case reports of fatal hepatic failure in offspring of women who used valproate during pregnancy.
Animal
In developmental toxicity studies conducted in mice, rats, rabbits, and monkeys, increased rates of fetal structural abnormalities, intrauterine growth retardation, and embryo-fetal death occurred following administration of valproate to pregnant animals during organogenesis at clinically relevant doses (calculated on a body surface area [mg/m 2] basis). Valproate induced malformations of multiple organ systems, including skeletal, cardiac, and urogenital defects. In mice, in addition to other malformations, fetal neural tube defects have been reported following valproate administration during critical periods of organogenesis, and the teratogenic response correlated with peak maternal drug levels. Behavioral abnormalities (including cognitive, locomotor, and social interaction deficits) and brain histopathological changes have also been reported in mice and rat offspring exposed prenatally to clinically relevant doses of valproate.
8.2 Lactation
Risk Summary
Valproate is excreted in human milk. Data in the published literature describe the presence of valproate in human milk (range: 0.4 mcg/mL to 3.9 mcg/mL), corresponding to 1% to 10% of maternal serum levels. Valproate serum concentrations collected from breastfed infants aged 3 days postnatal to 12 weeks following delivery ranged from 0.7 mcg/mL to 4 mcg/mL, which were 1% to 6% of maternal serum valproate levels. A published study in children up to six years of age did not report adverse developmental or cognitive effects following exposure to valproate via breast milk [see Data (Human)] .
There are no data to assess the effects of divalproex sodium on milk production or excretion.
Clinical Considerations
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for divalproex sodium and any potential adverse effects on the breastfed infant from divalproex sodium or from the underlying maternal condition.
Monitor the breastfed infant for signs of liver damage including jaundice and unusual bruising or bleeding. There have been reports of hepatic failure and clotting abnormalities in offspring of women who used valproate during pregnancy [see Use in Specific Populations ( 8.1)] .
Data
Human
In a published study, breast milk and maternal blood samples were obtained from 11 epilepsy patients taking valproate at doses ranging from 300 mg/day to 2,400 mg/day on postnatal days 3 to 6. In 4 patients who were taking valproate only, breast milk contained an average valproate concentration of 1.8 mcg/mL (range: 1.1 mcg/mL to 2.2 mcg/mL), which corresponded to 4.8% of the maternal plasma concentration (range: 2.7% to 7.4%). Across all patients (7 of whom were taking other AEDs concomitantly), similar results were obtained for breast milk concentration (1.8 mcg/mL, range: 0.4 mcg/mL to 3.9 mcg/mL) and maternal plasma ratio (5.1%, range: 1.3% to 9.6%).
A published study of 6 breastfeeding mother-infant pairs measured serum valproate levels during maternal treatment for bipolar disorder (750 mg/day or 1,000 mg/day). None of the mothers received valproate during pregnancy, and infants were aged from 4 weeks to 19 weeks at the time of evaluation. Infant serum levels ranged from 0.7 mcg/mL to 1.5 mcg/mL. With maternal serum valproate levels near or within the therapeutic range, infant exposure was 0.9% to 2.3% of maternal levels. Similarly, in 2 published case reports with maternal doses of 500 mg/day or 750 mg/day during breastfeeding of infants aged 3 months and 1 month, infant exposure was 1.5% and 6% that of the mother, respectively.
A prospective observational multicenter study evaluated the long-term neurodevelopmental effects of AED use on children. Pregnant women receiving monotherapy for epilepsy were enrolled with assessments of their children at ages 3 years and 6 years. Mothers continued AED therapy during the breastfeeding period. Adjusted IQs measured at 3 years for breastfed and non- breastfed children were 93 (n=11) and 90 (n=24), respectively. At 6 years, the scores for breastfed and non-breastfed children were 106 (n=11) and 94 (n=25), respectively (p=0.04). For other cognitive domains evaluated at 6 years, no adverse cognitive effects of continued exposure to an AED (including valproate) via breast milk were observed.
8.3 Females and Males of Reproductive Potential
Contraception
Women of childbearing potential should use effective contraception while taking valproate [see Boxed Warning, Warnings and Precautions ( 5.4), Drug Interactions ( 7), and Use in Specific Populations ( 8.1)] . This is especially important when valproate use is considered for a condition not usually associated with permanent injury or death such as prophylaxis of migraine headaches [see Contraindications ( 4)] .
Infertility
There have been reports of male infertility coincident with valproate therapy [see Adverse Reactions ( 6.4)].
In animal studies, oral administration of valproate at clinically relevant doses resulted in adverse reproductive effects in males [see Nonclinical Toxicology ( 13.1)] .
8.4 Pediatric Use
Experience with oral valproate has indicated that pediatric patients under the age of two years are at a considerably increased risk of developing fatal hepatotoxicity, especially those with the aforementioned conditions [see Boxed Warning] . The safety of Valproate Sodium Injection has not been studied in individuals below the age of 2 years. If a decision is made to use Valproate Sodium Injection in this age group, it should be used with extreme caution and as a sole agent. The benefits of therapy should be weighed against the risks. Above the age of 2 years, experience in epilepsy has indicated that the incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups.
Younger children, especially those receiving enzyme-inducing drugs, will require larger maintenance doses to attain targeted total and unbound valproate concentrations.
The variability in free fraction limits the clinical usefulness of monitoring total serum valproic acid concentrations. Interpretation of valproic acid concentrations in children should include consideration of factors that affect hepatic metabolism and protein binding.
Pediatric Clinical Trials
No unique safety concerns were identified in the 35 patients age 2 to 17 years who received Valproate Sodium Injection in clinical trials.
One twelve-month study was conducted to evaluate the safety of divalproex sodium sprinkle capsules in the indication of partial seizures (169 patients aged 3 to 10 years). The safety and tolerability of divalproex sodium in pediatric patients were shown to be comparable to those in adults [see Adverse Reactions ( 6)] .
Juvenile Animal Toxicology
In studies of valproate in immature animals, toxic effects not observed in adult animals included retinal dysplasia in rats treated during the neonatal period (from postnatal day 4) and nephrotoxicity in rats treated during the neonatal and juvenile (from postnatal day 14) periods. The no-effect dose for these findings was less than the maximum recommended human dose on a mg/m 2basis.
8.5 Geriatric Use
No patients above the age of 65 years were enrolled in double-blind prospective clinical trials of mania associated with bipolar illness. In a case review study of 583 patients, 72 patients (12%) were greater than 65 years of age. A higher percentage of patients above 65 years of age reported accidental injury, infection, pain, somnolence, and tremor. Discontinuation of valproate was occasionally associated with the latter two events. It is not clear whether these events indicate additional risk or whether they result from preexisting medical illness and concomitant medication use among these patients.
A study of elderly patients with dementia revealed drug related somnolence and discontinuation for somnolence [see Warnings and Precautions ( 5.13)] . The starting dose should be reduced in these patients, and dosage reductions or discontinuation should be considered in patients with excessive somnolence [see Dosage and Administration ( 2.2)] .
No unique safety concerns were identified in the 21 patients > 65 years of age receiving Valproate Sodium Injection in clinical trials.
- Pregnancy: Valproate Sodium Injection can cause congenital malformations including neural tube defects, decreased IQ, and neurodevelopmental disorders ( 5.2, 5.3, 8.1)
- Pediatric: Children under the age of two years are at considerably higher risk of fatal hepatotoxicity ( 5.1, 8.4)
- Geriatric: Reduce starting dose, increase dosage more slowly; monitor fluid and nutritional intake, and somnolence ( 5.13, 8.5)
OVERDOSAGE SECTION
10 OVERDOSAGE
Overdosage with valproate may result in somnolence, heart block, deep coma and hypernatremia. Fatalities have been reported; however patients have recovered from valproate serum concentrations as high as 2120 mcg/mL.
In overdose situations, the fraction of drug not bound to protein is high and hemodialysis or tandem hemodialysis plus hemoperfusion may result in significant removal of drug. General supportive measures should be applied with particular attention to the maintenance of adequate urinary output.
Naloxone has been reported to reverse the CNS depressant effects of valproate overdosage. Because naloxone could theoretically also reverse the antiepileptic effects of valproate, it should be used with caution in patients with epilepsy.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Valproate sodium exists as the valproate ion in the blood. The mechanisms by which valproate exerts its therapeutic effects have not been established. It has been suggested that its activity in epilepsy is related to increased brain concentrations of gamma-aminobutyric acid (GABA).
12.2 Pharmacodynamics
The relationship between plasma concentration and clinical response is not well documented. One contributing factor is the nonlinear, concentration dependent protein binding of valproate which affects the clearance of the drug. Thus, monitoring of total serum valproate cannot provide a reliable index of the bioactive valproate species.
For example, because the plasma protein binding of valproate is concentration dependent, the free fraction increases from approximately 10% at 40 mcg/mL to 18.5% at 130 mcg/mL. Higher than expected free fractions occur in the elderly, in hyperlipidemic patients, and in patients with hepatic and renal diseases.
Epilepsy
The therapeutic range in epilepsy is commonly considered to be 50 to 100 mcg/mL of total valproate, although some patients may be controlled with lower or higher plasma concentrations.
Equivalent doses of Valproate Sodium Injection and divalproex sodium yield equivalent plasma levels of the valproate ion [see Clinical Pharmacology ( 12.3)] .
12.3 Pharmacokinetics
Bioavailability
Equivalent doses of intravenous (IV) valproate and oral valproate products are expected to result in equivalent C max, C min, and total systemic exposure to the valproate ion when the IV valproate is administered as a 60 minute infusion. However, the rate of valproate ion absorption may vary with the formulation used. These differences should be of minor clinical importance under the steady state conditions achieved in chronic use in the treatment of epilepsy.
Administration of divalproex sodium tablets and IV valproate (given as a one hour infusion), 250 mg every 6 hours for 4 days to 18 healthy male volunteers resulted in equivalent AUC, C max, C minat steady state, as well as after the first dose. The T maxafter IV Valproate Sodium Injection occurs at the end of the one hour infusion, while the T maxafter oral dosing with divalproex sodium occurs at approximately 4 hours. Because the kinetics of unbound valproate are linear, bioequivalence between Valproate Sodium Injection and divalproex sodium up to the maximum recommended dose of 60 mg/kg/day can be assumed. The AUC and C maxresulting from administration of IV valproate 500 mg as a single one hour infusion and a single 500 mg dose of valproic acid syrup to 17 healthy male volunteers were also equivalent.
Patients maintained on valproic acid doses of 750 mg to 4250 mg daily (given in divided doses every 6 hours) as oral divalproex sodium alone (n = 24) or with another stabilized antiepileptic drug [carbamazepine (n = 15), phenytoin (n = 11), or phenobarbital (n = 1)], showed comparable plasma levels for valproic acid when switching from oral divalproex sodium to IV valproate (1-hour infusion).
Eleven healthy volunteers were given single infusions of 1000 mg IV valproate over 5, 10, 30, and 60 minutes in a 4-period crossover study. Total valproate concentrations were measured; unbound concentrations were not measured. After the 5 minute infusions (mean rate of 2.8 mg/kg/min), mean C maxwas 145 ± 32 mcg/mL, while after the 60 minute infusions, mean C maxwas 115 ± 8 mcg/mL. Ninety to 120 minutes after infusion initiation, total valproate concentrations were similar for all 4 rates of infusion. Because protein binding is nonlinear at higher total valproate concentrations, the corresponding increase in unbound C maxat faster infusion rates will be greater.
Distribution
Protein Binding
The plasma protein binding of valproate is concentration dependent and the free fraction increases from approximately 10% at 40 mcg/mL to 18.5% at 130 mcg/mL. Protein binding of valproate is reduced in the elderly, in patients with chronic hepatic diseases, in patients with renal impairment, and in the presence of other drugs (e.g., aspirin). Conversely, valproate may displace certain protein-bound drugs (e.g., phenytoin, carbamazepine, warfarin, and tolbutamide) (see Drug Interactions ( 7.2) for more detailed information on the pharmacokinetic interactions of valproate with other drugs).
CNS Distribution
Valproate concentrations in cerebrospinal fluid (CSF) approximate unbound concentrations in plasma (about 10% of total concentration).
Metabolism
Valproate is metabolized almost entirely by the liver. In adult patients on monotherapy, 30 to 50% of an administered dose appears in urine as a glucuronide conjugate. Mitochondrial β-oxidation is the other major metabolic pathway, typically accounting for over 40% of the dose. Usually, less than 15 to 20% of the dose is eliminated by other oxidative mechanisms. Less than 3% of an administered dose is excreted unchanged in urine.
The relationship between dose and total valproate concentration is nonlinear; concentration does not increase proportionally with the dose, but rather, increases to a lesser extent due to saturable plasma protein binding. The kinetics of unbound drug are linear.
Elimination
Mean plasma clearance and volume of distribution for total valproate are 0.56 L/hr/1.73 m 2and 11 L/1.73 m 2, respectively. Mean terminal half-life for valproate monotherapy after an intravenous infusion of 1,000 mg was 16 ± 3.0 hours.
The estimates cited apply primarily to patients who are not taking drugs that affect hepatic metabolizing enzyme systems. For example, patients taking enzyme-inducing antiepileptic drugs (carbamazepine, phenytoin, and phenobarbital) will clear valproate more rapidly. Because of these changes in valproate clearance, monitoring of antiepileptic concentrations should be intensified whenever concomitant antiepileptics are introduced or withdrawn.
Special Populations
Effect of Age
Neonates
Children within the first two months of life have a markedly decreased ability to eliminate valproate compared to older children and adults. This is a result of reduced clearance (perhaps due to delay in development of glucuronosyltransferase and other enzyme systems involved in valproate elimination) as well as increased volume of distribution (in part due to decreased plasma protein binding). For example, in one study, the half-life in children under 10 days ranged from 10 to 67 hours compared to a range of 7 to 13 hours in children greater than 2 months.
Children
Pediatric patients (i.e., between 3 months and 10 years) have 50% higher clearances expressed on weight (i.e., mL/min/kg) than do adults. Over the age of 10 years, children have pharmacokinetic parameters that approximate those of adults.
Elderly
The capacity of elderly patients (age range: 68 to 89 years) to eliminate valproate has been shown to be reduced compared to younger adults (age range: 22 to 26 years). Intrinsic clearance is reduced by 39%; the free fraction is increased by 44%. Accordingly, the initial dosage should be reduced in the elderly [see Dosage and Administration ( 2.2)] .
Effect of Sex
There are no differences in the body surface area adjusted unbound clearance between males and females (4.8 ± 0.17 and 4.7 ± 0.07 L/hr per 1.73 m 2, respectively).
Effect of Race
The effects of race on the kinetics of valproate have not been studied.
Effect of Disease
Liver Disease
Liver disease impairs the capacity to eliminate valproate. In one study, the clearance of free valproate was decreased by 50% in 7 patients with cirrhosis and by 16% in 4 patients with acute hepatitis, compared with 6 healthy subjects. In that study, the half-life of valproate was increased from 12 to 18 hours. Liver disease is also associated with decreased albumin concentrations and larger unbound fractions (2 to 2.6 fold increase) of valproate. Accordingly, monitoring of total concentrations may be misleading since free concentrations may be substantially elevated in patients with hepatic disease whereas total concentrations may appear to be normal [see Boxed Warning, Contraindications ( 4), and Warnings and Precautions ( 5.1)] .
Renal Disease
A slight reduction (27%) in the unbound clearance of valproate has been reported in patients with renal failure (creatinine clearance < 10 mL/minute); however, hemodialysis typically reduces valproate concentrations by about 20%. Therefore, no dosage adjustment appears to be necessary in patients with renal failure. Protein binding in these patients is substantially reduced; thus, monitoring total concentrations may be misleading.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Hepatotoxicity
Warn patients and guardians that nausea, vomiting, abdominal pain, anorexia, diarrhea, asthenia, and/or jaundice can be symptoms of hepatotoxicity and, therefore, require further medical evaluation promptly [see Warnings and Precautions ( 5.1)] .
Pancreatitis
Warn patients and guardians that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis and, therefore, require further medical evaluation promptly [see Warnings and Precautions ( 5.5)] .
Birth Defects and Decreased IQ
Inform pregnant women and women of childbearing potential (including girls beginning the onset of puberty) that use of valproate during pregnancy increases the risk of birth defects, decreased IQ, and neurodevelopmental disorders in children who were exposed in utero.
Advise women to use effective contraception while using valproate. When appropriate, counsel these patients about alternative therapeutic options. This is particularly important when valproate use is considered for a condition not usually associated with permanent injury or death such as prophylaxis of migraine headache [see Contraindications ( 4), Warnings and Precautions ( 5.2, 5.3, 5.4) and Use in Specific Populations ( 8.1)] .
Pregnancy Registry
Advise women of childbearing potential to discuss pregnancy planning with their doctor and to contact their doctor immediately if they think they are pregnant.
Encourage women who are taking valproate to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334 or visit the website, http://www.aedpregnancyregistry.org/ [see Use in Specific Populations ( 8.1)] .
Hyperammonemia
Inform patients of the signs and symptoms associated with hyperammonemic encephalopathy and to notify the prescriber if any of these symptoms occur [see Warnings and Precautions ( 5.8, 5.9)] .
CNS Depression
Since valproate products may produce CNS depression, especially when combined with another CNS depressant (e.g., alcohol), advise patients not to engage in hazardous activities, such as driving an automobile or operating dangerous machinery, until it is known that they do not become drowsy from the drug.
Multi-Organ Hypersensitivity Reactions
Instruct patients that a fever associated with other organ system involvement (rash, lymphadenopathy, etc.) may be drug-related and should be reported to the physician immediately [see Warnings and Precautions ( 5.11)] .
Athenex
****Mfd. for Athenex
Schaumburg, IL 60173 (USA)
Made in India
©2022 Athenex.
May 2022
REFERENCES SECTION
15 REFERENCES
- Meador KJ, Baker GA, Browning N, et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurology 2013; 12 (3):244-252.
DESCRIPTION SECTION
11 DESCRIPTION
Valproate sodium is the sodium salt of valproic acid designated as sodium 2-propylpentanoate. Valproate sodium has the following structure:
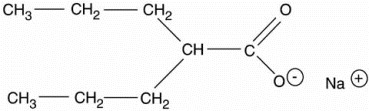
Valproate sodium has a molecular weight of 166.2. It occurs as an essentially white and odorless, crystalline, deliquescent powder.
Valproate Sodium Injection, USP is available in 5 mL single-dose vials for intravenous injection. Each mL contains valproate sodium equivalent to 100 mg valproic acid, edetate disodium 0.40 mg, and water for injection to volume. The pH is adjusted to 7.6 with sodium hydroxide and/or hydrochloric acid. The solution is clear and colorless.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, and Impairment of Fertility
Carcinogenesis
Valproate was administered orally to rats and mice at doses of 80 and 170 mg/kg/day (less than the maximum recommended human dose on a mg/m 2basis) for two years. The primary findings were an increase in the incidence of subcutaneous fibrosarcomas in high-dose male rats receiving valproate and a dose-related trend for benign pulmonary adenomas in male mice receiving valproate.
Mutagenesis
Valproate was not mutagenic in an in vitrobacterial assay (Ames test), did not produce dominant lethal effects in mice, and did not increase chromosome aberration frequency in an in vivocytogenetic study in rats. Increased frequencies of sister chromatid exchange (SCE) have been reported in a study of epileptic children taking valproate; this association was not observed in another study conducted in adults.
Impairment of Fertility
In chronic toxicity studies in juvenile and adult rats and dogs, administration of valproate resulted in testicular atrophy and reduced spermatogenesis at oral doses of 400 mg/kg/day or greater in rats (approximately equal to or greater than the maximum recommended human dose (MRHD) on a mg/m 2basis) and 150 mg/kg/day or greater in dogs (approximately equal to or greater than the MRHD on a mg/m 2basis). Fertility studies in rats have shown no effect on fertility at oral doses of valproate up to 350 mg/kg/day (approximately equal to the MRHD on a mg/m 2basis) for 60 days.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
The studies described in the following section were conducted with oral divalproex sodium tablets.
14.1 Epilepsy
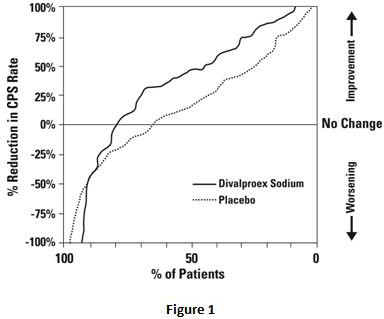
The efficacy of valproate in reducing the incidence of complex partial seizures (CPS) that occur in isolation or in association with other seizure types was established in two controlled trials.
In one, multi-clinic, placebo controlled study employing an add-on design (adjunctive therapy), 144 patients who continued to suffer eight or more CPS per 8 weeks during an 8 week period of monotherapy with doses of either carbamazepine or phenytoin sufficient to assure plasma concentrations within the “therapeutic range” were randomized to receive, in addition to their original antiepilepsy drug (AED), either divalproex sodium or placebo. Randomized patients were to be followed for a total of 16 weeks. The following table presents the findings.
Table 4. Adjunctive Therapy Study Median Incidence of CPS per 8 Weeks
| |||
|
Add-on Treatment |
Number of Patients |
Baseline Incidence |
Experimental Incidence |
|
Divalproex sodium |
75 |
16.0 |
8.9* |
|
Placebo |
69 |
14.5 |
11.5 |
Figure 1presents the proportion of patients (X axis) whose percentage reduction from baseline in complex partial seizure rates was at least as great as that indicated on the Y axis in the adjunctive therapy study. A positive percent reduction indicates an improvement (i.e., a decrease in seizure frequency), while a negative percent reduction indicates worsening. Thus, in a display of this type, the curve for an effective treatment is shifted to the left of the curve for placebo. This figure shows that the proportion of patients achieving any particular level of improvement was consistently higher for valproate than for placebo. For example, 45% of patients treated with valproate had a ≥ 50% reduction in complex partial seizure rate compared to 23% of patients treated with placebo.
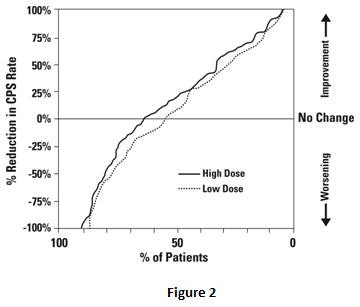
The second study assessed the capacity of valproate to reduce the incidence of CPS when administered as the sole AED. The study compared the incidence of CPS among patients randomized to either a high or low dose treatment arm. Patients qualified for entry into the randomized comparison phase of this study only if
- they continued to experience 2 or more CPS per 4 weeks during an 8 to 12 week long period of monotherapy with adequate doses of an AED (i.e., phenytoin, carbamazepine, phenobarbital, or primidone) and 2) they made a successful transition over a two week interval to valproate. Patients entering the randomized phase were then brought to their assigned target dose, gradually tapered off their concomitant AED and followed for an interval as long as 22 weeks. Less than 50% of the patients randomized, however, completed the study. In patients converted to divalproex sodium monotherapy, the mean total valproate concentrations during monotherapy were 71 and 123 mcg/mL in the low dose and high dose groups, respectively.
The following table presents the findings for all patients randomized who had at least one post-randomization assessment.
Table 5. Monotherapy Study Median Incidence of CPS per 8 Weeks
| |||
|
Treatment |
Number of Patients |
Baseline Incidence |
Randomized Phase Incidence |
|
High dose divalproex sodium |
131 |
13.2 |
10.7* |
|
Low dose divalproex sodium |
134 |
14.2 |
13.8 |
Figure 2presents the proportion of patients (X axis) whose percentage reduction from baseline in complex partial seizure rates was at least as great as that indicated on the Y axis in the monotherapy study. A positive percent reduction indicates an improvement (i.e., a decrease in seizure frequency), while a negative percent reduction indicates worsening. Thus, in a display of this type, the curve for a more effective treatment is shifted to the left of the curve for a less effective treatment. This figure shows that the proportion of patients achieving any particular level of reduction was consistently higher for high dose valproate than for low dose valproate. For example, when switching from carbamazepine, phenytoin, phenobarbital or primidone monotherapy to high dose valproate monotherapy, 63% of patients experienced no change or a reduction in complex partial seizure rates compared to 54% of patients receiving low dose valproate.
Information on pediatric studies is presented in section 8.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Valproate Sodium Injection, USP, equivalent to 100 mg of valproic acid per mL, is a clear, colorless solution and is supplied as follows:
|
NDC |
Valproate Sodium Injection, USP (100 mg per mL) |
Package Factor |
|
70860-784-05 |
500 mg per 5 mL Single-Dose Vial |
10 vials per carton |
Storage Conditions
Store vials at 20° to 25°C (68° to 77°F); excursions permitted between 15° and 30°C (59° and 86°F). [See USP Controlled Room Temperature.]
Discard unused portion.
Sterile, Nonpyrogenic, Preservative-free.
** The container closure is not made with natural rubber latex.**
