Calcium Acetate
These highlights do not include all the information needed to use Calcium Acetate Capsules safely and effectively. See full prescribing information for Calcium Acetate Capsules. Calcium Acetate capsules, for oral use Initial U.S. Approval: 1990
a23b6070-eb4b-48e3-b563-8232206a6be4
HUMAN PRESCRIPTION DRUG LABEL
Jun 25, 2025
Cardinal Health 107, LLC
DUNS: 118546603
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Calcium Acetate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (17)
Drug Labeling Information
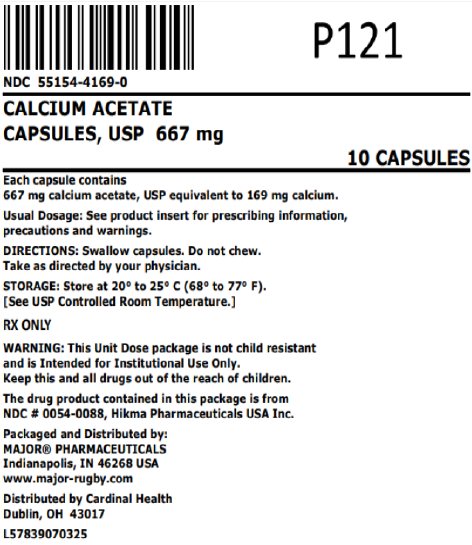
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Package/Label Display Panel
NDC 55154-4169-0
CALCIUM ACETATE
CAPSULES, USP 667 mg
10 CAPSULES
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
Hypercalcemia is discussed elsewhere [see Warnings and Precautions (5.1)].
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical studies, calcium acetate has been generally well tolerated.
Calcium acetate was studied in a 3 month, open-label, non-randomized study of 98 enrolled ESRD hemodialysis patients and an alternate liquid formulation of calcium acetate was studied in a two week double-blind, placebo-controlled, cross-over study with 69 enrolled ESRD hemodialysis patients. Adverse reactions (>2% on treatment) from these trials are presented in Table 1.
Table 1: Adverse Reactions in Patients with End-Stage Renal Disease Undergoing Hemodialysis|
Preferred Term |
Total adverse reactions reported for calcium acetate N=167 N (%) |
3 month, open label study of calcium acetate N=98 N (%) |
Double blind, placebo-controlled, cross-over study of liquid calcium acetate N=69 | |
|
Calcium acetate N (%) |
Placebo N (%) | |||
|
Nausea |
6 (3.6) |
6 (6.1) |
0 (0.0) |
0 (0.0) |
|
Vomiting |
4 (2.4) |
4 (4.1) |
0 (0.0) |
0 (0.0) |
|
Hypercalcemia |
21 (12.6) |
16 (16.3) |
5 (7.2) |
0 (0.0) |
Mild hypercalcemia may be asymptomatic or manifest itself as constipation, anorexia, nausea, and vomiting. More severe hypercalcemia is associated with confusion, delirium, stupor, and coma. Decreasing dialysate calcium concentration could reduce the incidence and severity of calcium acetate**-**induced hypercalcemia. Isolated cases pruritus have been reported, which may represent allergic reactions.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency or to establish a causal relationship to drug exposure.
The following additional adverse reactions have been identified during post- approval of calcium acetate: dizziness, edema, and weakness.
•
The most common (>10%) adverse reactions are hypercalcemia, nausea and vomiting. (6.1)
•
In clinical studies, patients have occasionally experienced nausea during calcium acetate therapy. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-800-962-8364 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Calcium Acetate Capsules, USP
667 mg capsule is supplied as a white opaque/blue opaque capsule, imprinted with “54 215” on the cap and body.
Overbagged with 10 capsules per bag, NDC 55154-4169-0
WARNING: These Unit Dose packages are not child resistant and are Intended for Institutional Use Only. Keep this and all drugs out of the reach of children.
Storage
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Inform patients to take calcium acetate capsules with meals, adhere to their prescribed diets, and avoid the use of calcium supplements including nonprescription antacids. Inform the patients about the symptoms of hypercalcemia [see Warnings and Precautions (5.1)and Adverse Reactions (6.1)].
Advise patients who are taking an oral medication where reduction in the bioavailability of that medication would have clinically significant effect on its safety or efficacy to take the drug one hour before or three hours after calcium acetate capsules.
Distr. by:** Hikma**
Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
Packaged and Distributed by:
MAJOR® PHARMACEUTICALS
Indianapolis, IN 46268 USA
Refer to package label for Distributor's NDC Number
Distributed By:
Cardinal Health
Dublin, OH 43017
L57839070325
C50000408/01
Revised September 2020
DESCRIPTION SECTION
11 DESCRIPTION
Calcium acetate acts as a phosphate binder. Its chemical name is calcium acetate. Its molecular formula is C4H6CaO4, and its molecular weight is 158.17. Its structural formula is:

Each white opaque/blue opaque capsule contains 667 mg of calcium acetate, USP (anhydrous; Ca(CH3COO)2; MW=158.17 grams) equal to 169 mg (8.45 mEq) calcium, polyethylene glycol 8000 and magnesium stearate. Each capsule shell contains: black monogramming ink, FD&C Blue #1, FD&C Red #3, gelatin and titanium dioxide. The black monogramming ink contains: ammonium hydroxide, iron oxide black, isopropyl alcohol, n-butyl alcohol, propylene glycol and shellac glaze.
Calcium Acetate Capsules, USP are administered orally for the control of hyperphosphatemia in end-stage renal failure.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
Effectiveness of calcium acetate in decreasing serum phosphorus has been demonstrated in two studies of the calcium acetate solid oral dosage form.
Ninety-one patients with end-stage renal disease who were undergoing hemodialysis and were hyperphosphatemic (serum phosphorus >5.5 mg/dL) following a 1 week phosphate binder washout period contributed efficacy data to an open-label, non-randomized study.
The patients received calcium acetate 667 mg tablets at each meal for a period of 12 weeks. The initial starting dose was 2 tablets per meal for 3 meals a day, and the dose was adjusted as necessary to control serum phosphorus levels. The average final dose after 12 weeks of treatment was 3.4 tablets per meal. Although there was a decrease in serum phosphorus, in the absence of a control group the true magnitude of effect is uncertain.
The data presented in Table 2 demonstrate the efficacy of calcium acetate in the treatment of hyperphosphatemia in end-stage renal disease patients. The effects on serum calcium levels are also presented.
Table 2: Average Serum Phosphorous and Calcium Levels at Pre-Study, Interim, and Study Completion Time Points
| |||||
|
Parameter |
Pre-Study |
Week 4* |
Week 8 |
Week 12 |
p-value† |
|
Phosphorus (mg/dL)‡ |
7.4 ± 0.17 |
5.9 ± 0.16 |
5.6 ± 0.17 |
5.2 ± 0.17 |
≤0.01 |
|
Calcium (mg/dL)‡ |
8.9 ± 0.09 |
9.5 ± 0.10 |
9.7 ± 0.10 |
9.7 ± 0.10 |
≤0.01 |
There was a 30% decrease in serum phosphorus levels during the 12 week study period (p<0.01). Two-thirds of the decline occurred in the first month of the study. Serum calcium increased 9% during the study mostly in the first month of the study.
Treatment with the phosphate binder was discontinued for patients from the open-label study, and those patients whose serum phosphorus exceeded 5.5 mg/dL were eligible for entry into a double-blind, placebo-controlled, cross-over study. Patients were randomized to receive calcium acetate or placebo, and each continued to receive the same number of tablets as had been individually established during the previous study. Following 2 weeks of treatment, patients switched to the alternative therapy for an additional 2 weeks.
The phosphate binding effect of calcium acetate is shown in the Table 3.
Table 3: Serum Phosphorous and Calcium Levels at Study Initiation and After Completion of Each Treatment Arm
| ||||
|
Parameter |
Pre-Study |
Post-Treatment |
p-value* | |
|
Calcium Acetate |
Placebo | |||
|
Phosphorus (mg/dL)† |
7.3 ± 0.18 |
5.9 ± 0.24 |
7.8 ± 0.22 |
<0.01 |
|
Calcium (mg/dL)† |
8.9 ± 0.11 |
9.5 ± 0.13 |
8.8 ± 0.12 |
<0.01 |
Overall, 2 weeks of treatment with calcium acetate statistically significantly (p<0.01) decreased serum phosphorus by a mean of 19% and increased serum calcium by a statistically significant (p<0.01) but clinically unimportant mean of 7%.
