Eplerenone
These highlights do not include all the information needed to use EPLERENONE TABLETS safely and effectively. See full prescribing information for EPLERENONE TABLETS.EPLERENONE tablets, for oral useInitial U.S. Approval: 2002
cd6cbf0b-34b8-43aa-8037-360480a19cf8
HUMAN PRESCRIPTION DRUG LABEL
Sep 10, 2020
Eon Labs, Inc.
DUNS: 012656273
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Eplerenone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (13)
Eplerenone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (10)
Drug Labeling Information
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 CYP3A Inhibitors
Eplerenone metabolism is predominantly mediated via CYP3A. Do not use eplerenone with drugs that are strong inhibitors of CYP3A [see Contraindications (4)andClinical Pharmacology (12.3)].
In post-MI HFrEF patients taking a moderate CYP3A inhibitor, do not exceed 25 mg once daily. In patients with hypertension taking a moderate CYP3A inhibitor, initiate at 25 mg once daily. For inadequate blood pressure response, dosing may be increased to a maximum of 25 mg twice daily [see Dosage and Administration (2.3, 2.4)andClinical Pharmacology (12.3)].
7.2 ACE Inhibitors and Angiotensin II Receptor Antagonists
The risk of hyperkalaemia increase when eplerenone is used in combination with an ACE inhibitor and/or an ARB. A close monitoring of serum potassium and renal function is recommended, especially in patients at risk for impaired renal function, e.g., the elderly [see Warnings and Precautions (5.1)].
7.3 Lithium
A drug interaction study of eplerenone with lithium has not been conducted. Lithium toxicity has been reported in patients receiving lithium concomitantly with diuretics and ACE inhibitors. Serum lithium levels should be monitored frequently if eplerenone is administered concomitantly with lithium.
7.4 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
A drug interaction study of eplerenone with an NSAID has not been conducted. The administration of other potassium-sparing antihypertensives with NSAIDs has been shown to reduce the antihypertensive effect in some patients and result in severe hyperkalemia in patients with impaired renal function. Therefore, when eplerenone and NSAIDs are used concomitantly, monitor blood pressure and serum potassium levels.
•
CYP3A Inhibitors: In post-MI HFrEF patients do not exceed 25 mg once daily when used with moderate CYP3A inhibitors (e.g., verapamil, erythromycin, saquinavir, fluconazole). In patients with hypertension initiate at 25 mg once daily. For inadequate blood pressure response, dosing may be increased to a maximum of 25 mg twice daily. (2.4,7.1,12.3)
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Eplerenone was non-genotoxic in a battery of assays including in vitro bacterial mutagenesis (Ames test in Salmonella spp. and E. Coli), in vitro mammalian cell mutagenesis (mouse lymphoma cells), in vitro chromosomal aberration (Chinese hamster ovary cells), in vivo rat bone marrow micronucleus formation, and in vivo/ex vivo unscheduled DNA synthesis in rat liver.
There was no drug-related tumor response in heterozygous P53 deficient mice when tested for 6 months at dosages up to 1000 mg/kg/day (systemic AUC exposures up to 9 times the exposure in humans receiving the 100 mg/day therapeutic dose). Statistically significant increases in benign thyroid tumors were observed after 2 years in both male and female rats when administered eplerenone 250 mg/kg/day (highest dose tested) and in male rats only at 75 mg/kg/day. These dosages provided systemic AUC exposures approximately 2 to 12 times higher than the average human therapeutic exposure at 100 mg/day. Repeat dose administration of eplerenone to rats increases the hepatic conjugation and clearance of thyroxin, which results in increased levels of TSH by a compensatory mechanism. Drugs that have produced thyroid tumors by this rodent-specific mechanism have not shown a similar effect in humans.
Male rats treated with eplerenone at 1000 mg/kg/day for 10 weeks (AUC 17 times that at the 100 mg/day human therapeutic dose) had decreased weights of seminal vesicles and epididymides and slightly decreased fertility. Dogs administered eplerenone at dosages of 15 mg/kg/day and higher (AUC 5 times that at the 100 mg/day human therapeutic dose) had dose-related prostate atrophy. The prostate atrophy was reversible after daily treatment for 1 year at 100 mg/kg/day. Dogs with prostate atrophy showed no decline in libido, sexual performance, or semen quality. Testicular weight and histology were not affected by eplerenone in any test animal species at any dosage.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Heart Failure Post-Myocardial Infarction
The eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS) was a multinational, multicenter, double-blind, randomized, placebo-controlled study in patients clinically stable 3 to 14 days after an acute MI with LV dysfunction (as measured by left ventricular ejection fraction [LVEF] ≤40%) and either diabetes or clinical evidence of HF (pulmonary congestion by exam or chest x-ray or S3). Patients with HF of valvular or congenital etiology, patients with unstable post-infarct angina, and patients with serum potassium >5.0 mEq/L or serum creatinine >2.5 mg/dL were to be excluded. Patients were allowed to receive standard post-MI drug therapy and to undergo revascularization by angioplasty or coronary artery bypass graft surgery.
Patients randomized to eplerenone were given an initial dose of 25 mg once daily and titrated to the target dose of 50 mg once daily after 4 weeks if serum potassium was <5.0 mEq/L. Dosage was reduced or suspended anytime during the study if serum potassium levels were ≥5.5 mEq/L [see Dosage and Administration (2.1)].
EPHESUS randomized 6,632 patients (9.3% U.S.) at 671 centers in 27 countries. The study population was primarily white (90%, with 1% Black, 1% Asian, 6% Hispanic, 2% other) and male (71%). The mean age was 64 years (range, 22 to 94 years). The majority of patients had pulmonary congestion (75%) by exam or x-ray and were Killip Class II (64%). The mean ejection fraction was 33%. The average time to enrollment was 7 days post-MI. Medical histories prior to the index MI included hypertension (60%), coronary artery disease (62%), dyslipidemia (48%), angina (41%), type 2 diabetes (30%), previous MI (27%), and HF (15%).
The mean dose of eplerenone was 43 mg/day. Patients also received standard care including aspirin (92%), ACE inhibitors (90%), beta-blockers (83%), nitrates (72%), loop diuretics (66%), or HMG-CoA reductase inhibitors (60%).
Patients were followed for an average of 16 months (range, 0 to 33 months). The ascertainment rate for vital status was 99.7%.
The co-primary endpoints for EPHESUS were (1) the time to death from any cause, and (2) the time to first occurrence of either cardiovascular mortality [defined as sudden cardiac death or death due to progression of HF, stroke, or other CV causes] or CV hospitalization (defined as hospitalization for progression of HF, ventricular arrhythmias, acute MI, or stroke).
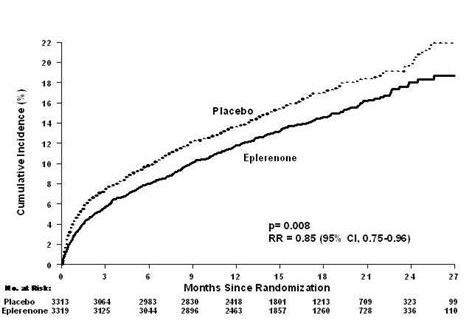
For the co-primary endpoint for death from any cause, there were 478 deaths in the eplerenone group (14.4%) and 554 deaths in the placebo group (16.7%). The risk of death with eplerenone was reduced by 15% [hazard ratio equal to 0.85 (95% confidence interval 0.75 to 0.96; p=0.008 by log rank test)]. Kaplan- Meier estimates of all-cause mortality are shown inFigure 1 and the components of mortality are provided inTable 5.
Figure 1. Kaplan-Meier Estimates of All-Cause Mortality
|
Eplerenone (N=3,319) n (%) |
Placebo (N=3,313) n (%) |
Hazard Ratio |
p-value | |
|
Death from any cause |
478 (14.4) |
554 (16.7) |
0.85 |
0.008 |
|
CV Death |
407 (12.3) |
483 (14.6) |
0.83 |
0.005 |
|
Non-CV Death |
60 (1.8) |
54 (1.6) | ||
|
Unknown or unwitnessed death |
11 (0.3) |
17 (0.5) |
Most CV deaths were attributed to sudden death, acute MI, and HF.
The time to first event for the co-primary endpoint of CV death or hospitalization, as defined above, was longer in the eplerenone group (hazard ratio 0.87, 95% confidence interval 0.79 to 0.95, p=0.002). An analysis that included the time to first occurrence of CV mortality and all CV hospitalizations (atrial arrhythmia, angina, CV procedures, progression of HF, MI, stroke, ventricular arrhythmia, or other CV causes) showed a smaller effect with a hazard ratio of 0.92 (95% confidence interval 0.86 to 0.99; p=0.028). The combined endpoints, including combined all-cause hospitalization and mortality were driven primarily by CV mortality. The combined endpoints in EPHESUS, including all-cause hospitalization and all-cause mortality, are presented inTable 6.
Table 6. Rates of Death or Hospitalization in EPHESUS
| ||
|
Event |
Eplerenone n (%) |
Placebo n (%) |
|
CV death or hospitalization for progression of HF, stroke, MI or ventricular arrhythmia* Death Hospitalization |
885 (26.7) 407 (12.3) 606 (18.3) |
993 (30.0) 483 (14.6) 649 (19.6) |
|
CV death or hospitalization for progression of HF, stroke, MI, ventricular arrhythmia, atrial arrhythmia, angina, CV procedures, or other CV causes (PVD; Hypotension) Death Hospitalization |
1,516 (45.7) 407 (12.3) 1,281 (38.6) |
1,610 (48.6) 483 (14.6) 1,307 (39.5) |
|
All-cause death or hospitalization Death* Hospitalization |
1,734 (52.2) 478 (14.4) 1,497 (45.1) |
1,833 (55.3) 554 (16.7) 1,530 (46.2) |
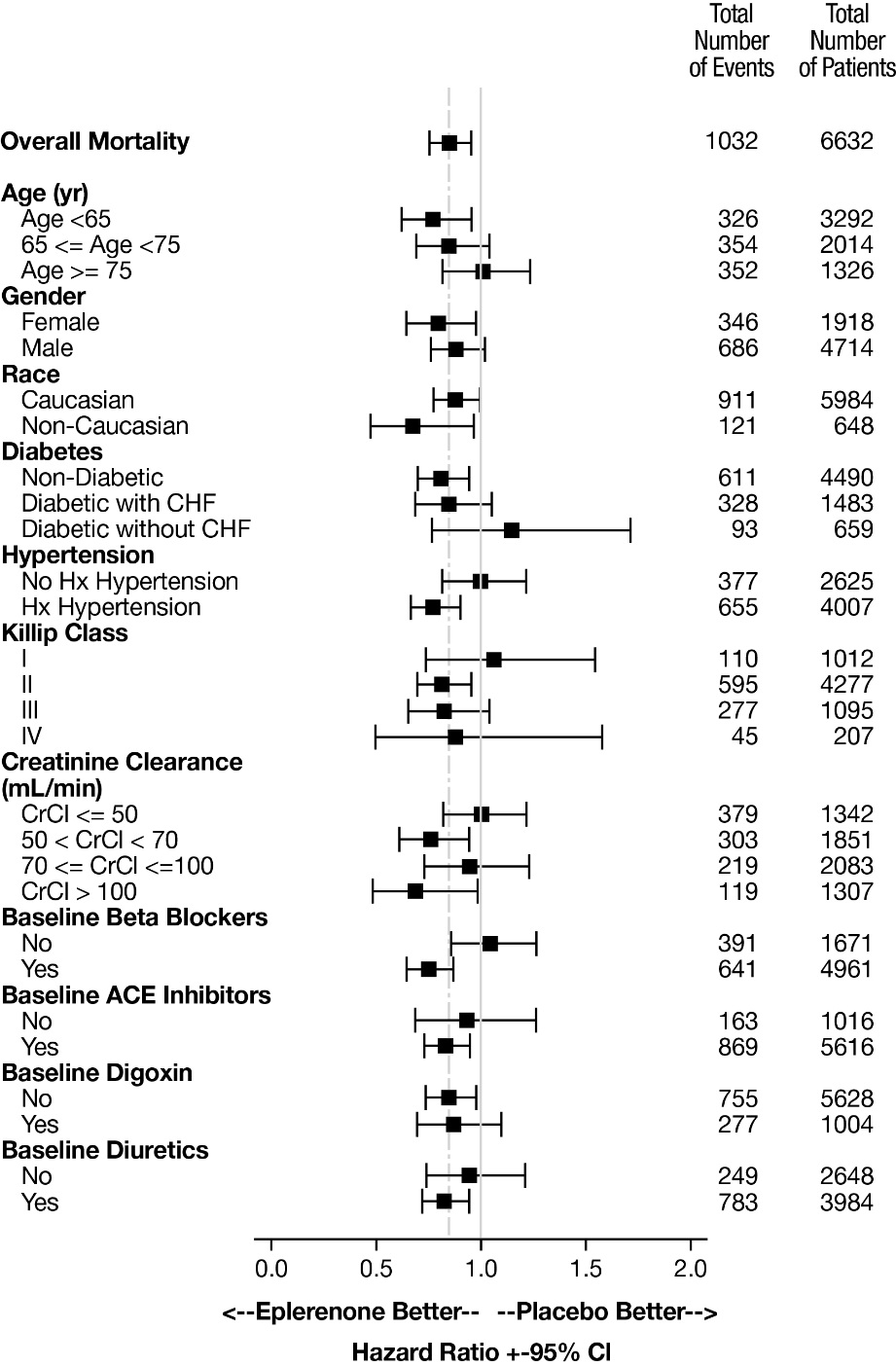
Mortality hazard ratios varied for some subgroups as shown inFigure 2. Mortality hazard ratios appeared favorable for eplerenone for both genders and for all races or ethnic groups, although the numbers of non-Caucasians were low (648, 10%). Patients with diabetes without clinical evidence of HF and patients greater than 75 years did not appear to benefit from the use of eplerenone. Such subgroup analyses must be interpreted cautiously.
Figure 2. Hazard Ratios of All-Cause Mortality by Subgroups
Analyses conducted for a variety of CV biomarkers did not confirm a mechanism of action by which mortality was reduced.
14.2 Hypertension
The safety and efficacy of eplerenone have been evaluated alone and in combination with other antihypertensive agents in clinical studies of 3091 hypertensive patients. The studies included 46% women, 14% Blacks, and 22% elderly (age ≥65). The studies excluded patients with elevated baseline serum potassium (>5.0 mEq/L) and elevated baseline serum creatinine (generally >1.5 mg/dL in males and >1.3 mg/dL in females).
Two fixed-dose, placebo-controlled, 8- to 12-week monotherapy studies in patients with baseline diastolic blood pressures of 95 mm Hg to 114 mm Hg were conducted to assess the antihypertensive effect of eplerenone. In these two studies, 611 patients were randomized to eplerenone and 140 patients to placebo. Patients received eplerenone in doses of 25 mg to 400 mg daily as either a single daily dose or divided into two daily doses. The mean placebo- subtracted reductions in trough cuff blood pressure achieved by eplerenone in these studies at doses up to 200 mg are shown inFigure 3 andFigure 4.
Figure 3. Eplerenone Dose Response-Trough Cuff SBP Placebo-Subtracted Adjusted Mean Change from Baseline in Hypertension Studies
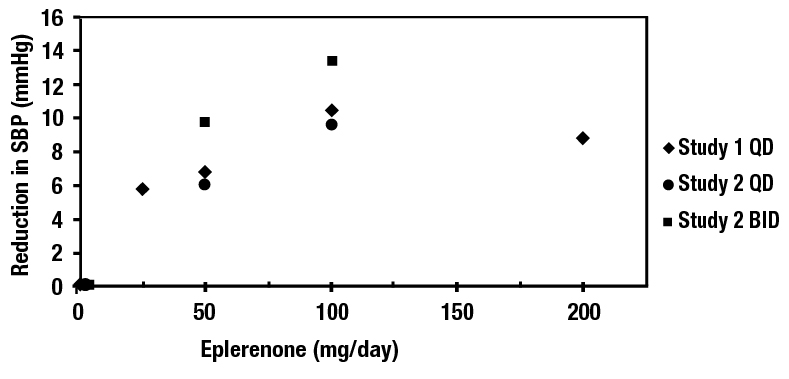
Figure 4. Eplerenone Dose Response-Trough Cuff DBP Placebo-Subtracted Adjusted Mean Change from Baseline in Hypertension Studies
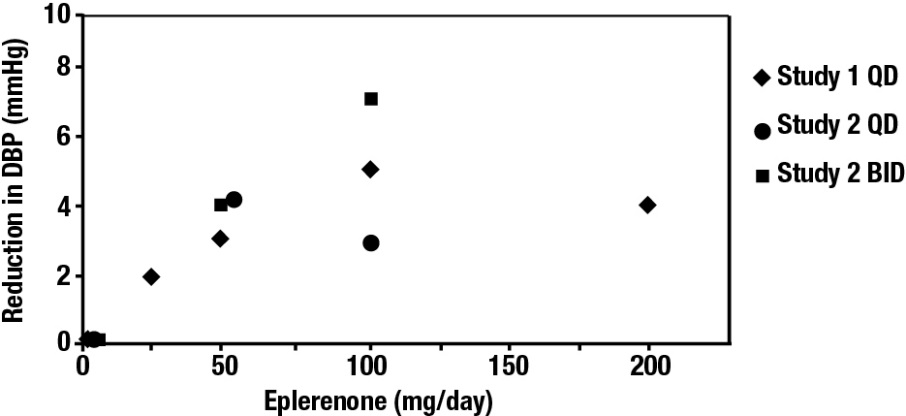
Patients treated with eplerenone 50 mg to 200 mg daily experienced significant decreases in sitting systolic and diastolic blood pressure at trough with differences from placebo of 6 mm Hg to 13 mm Hg (systolic) and 3 mm Hg to 7 mm Hg (diastolic). These effects were confirmed by assessments with 24-hour ambulatory blood pressure monitoring (ABPM). In these studies, assessments of 24-hour ABPM data demonstrated that eplerenone, administered once or twice daily, maintained antihypertensive efficacy over the entire dosing interval. However, at a total daily dose of 100 mg, eplerenone administered as 50 mg twice per day produced greater trough cuff (4/3 mm Hg) and ABPM (2/1 mm Hg) blood pressure reductions than 100 mg given once daily.
Blood pressure lowering was apparent within 2 weeks from the start of therapy with eplerenone, with maximal antihypertensive effects achieved within 4 weeks. Stopping eplerenone following treatment for 8 to 24 weeks in six studies did not lead to adverse event rates in the week following withdrawal of eplerenone greater than following placebo or active control withdrawal. Blood pressures in patients not taking other antihypertensives rose 1 week after withdrawal of eplerenone by about 6/3 mm Hg, suggesting that the antihypertensive effect of eplerenone was maintained through 8 to 24 weeks.
Blood pressure reductions with eplerenone in the two fixed-dose monotherapy studies and other studies using titrated doses, as well as concomitant treatments, were not significantly different when analyzed by age, gender, or race with one exception. In a study in patients with low renin hypertension, blood pressure reductions in Blacks were smaller than those in whites during the initial titration period with eplerenone.
Eplerenone has been studied concomitantly with treatment with ACE inhibitors, ARB, calcium channel blockers, beta-blockers, and hydrochlorothiazide. When administered concomitantly with one of these drugs eplerenone usually produced its expected antihypertensive effects.
