itraconazole
Itraconazole Capsules
6242b7ad-eaa0-a524-b6e0-ec33e63407db
HUMAN PRESCRIPTION DRUG LABEL
Mar 25, 2024
Patriot Pharmaceuticals
DUNS: 178220385
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
ITRACONAZOLE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
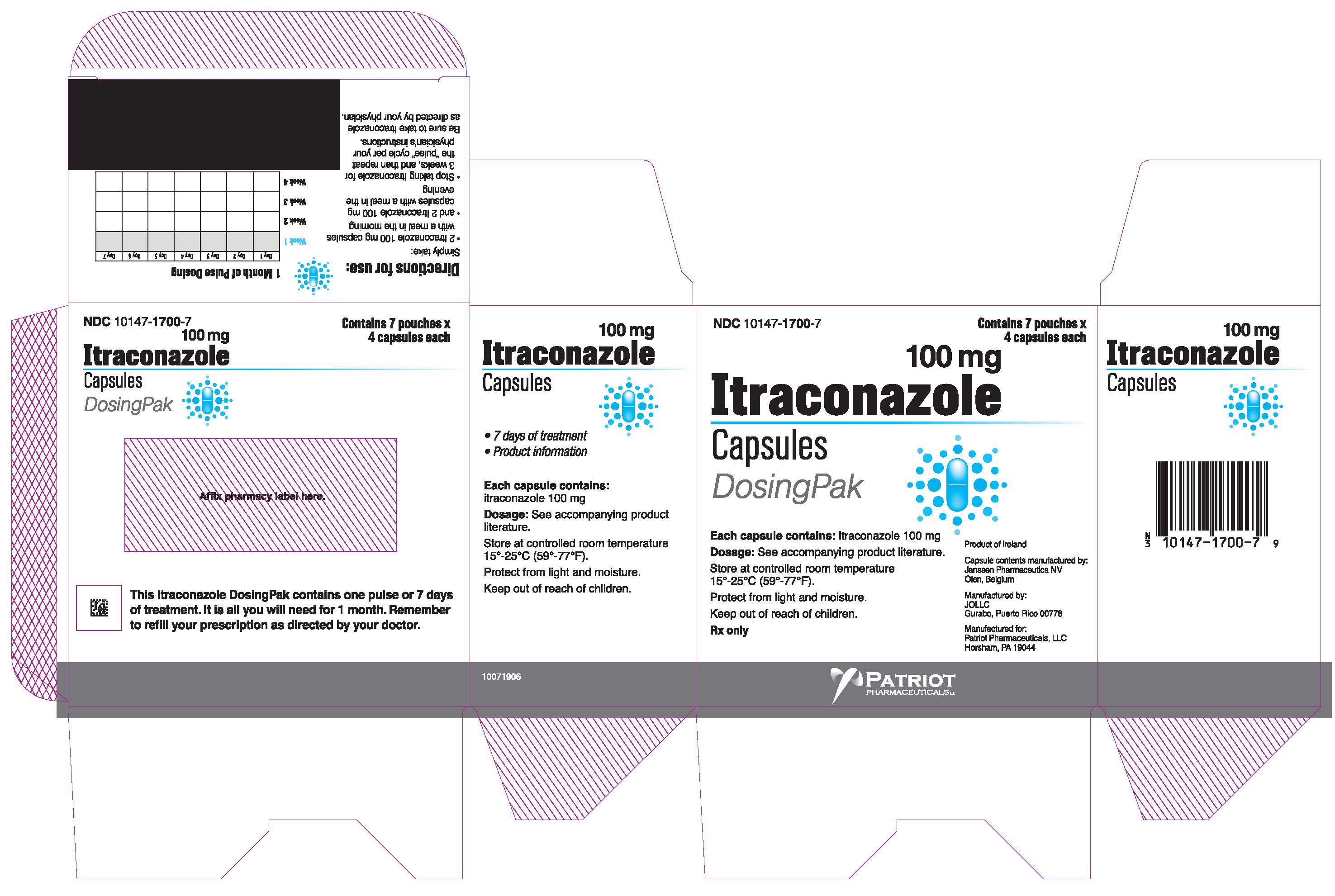
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 100 mg Carton
NDC 10147-1700-7
Contains 7 pouches x
** 4 capsules each**
100 mg
** Itraconazole**
Capsules
DosingPak
**Each capsule contains:**itraconazole 100 mg
**Dosage:**See accompanying product literature.
Store at controlled room temperature
15°-25°C (59°-77°F).
Protect from light and moisture.
Keep out of reach of children.
Rx only
Product of Ireland
Capsule contents manufactured by:
Janssen Pharmaceutica NV
Olen, Belgium
Manufactured by:
JOLLC
Gurabo, Puerto Rico 00778
Manufactured for:
Patriot Pharmaceuticals, LLC
Horsham, PA 19044, USA
PATRIOT
PHARMACEUTICALS LLC
BOXED WARNING SECTION
BOXED WARNING
Congestive Heart Failure, Cardiac Effects and Drug Interactions
Congestive Heart Failure and Cardiac Effects
Itraconazole Capsules should not be administered for the treatment of onychomycosis in patients with evidence of ventricular dysfunction such as congestive heart failure (CHF) or a history of CHF. If signs or symptoms of congestive heart failure occur during administration of Itraconazole Capsules, discontinue administration. When itraconazole was administered intravenously to dogs and healthy human volunteers, negative inotropic effects were seen. (See**CONTRAINDICATIONS**,WARNINGS,PRECAUTIONS: Drug Interactions,ADVERSE REACTIONS: Post-marketing Experience, andCLINICAL PHARMACOLOGY: Special Populationsfor more information.)**
Drug Interactions
Coadministration of a number of CYP3A4 substrates are contraindicated with Itraconazole Capsules. Some examples of drugs that are contraindicated for coadministration with Itraconazole Capsules are: methadone, disopyramide, dofetilide, dronedarone, quinidine, isavuconazole, ergot alkaloids (such as dihydroergotamine, ergometrine (ergonovine), ergotamine, methylergometrine (methylergonovine)), irinotecan, lurasidone, oral midazolam, pimozide, triazolam, felodipine, nisoldipine, ivabradine, ranolazine, eplerenone, cisapride, naloxegol, lomitapide, lovastatin, simvastatin, avanafil, ticagrelor, finerenone, voclosporin. Coadministration with colchicine, fesoterodine and solifenacin is contraindicated in subjects with varying degrees of renal or hepatic impairment. Coadministration with eliglustat is contraindicated in subjects that are poor or intermediate metabolizers of CYP2D6 and in subjects taking strong or moderate CYP2D6 inhibitors. Coadministration with venetoclax is contraindicated in patients with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) during the dose initiation and ramp-up phase of venetoclax. See**PRECAUTIONS: Drug InteractionsSection for specific examples. Coadministration with itraconazole can cause elevated plasma concentrations of these drugs and may increase or prolong both the pharmacologic effects and/or adverse reactions to these drugs. For example, increased plasma concentrations of some of these drugs can lead to QT prolongation and ventricular tachyarrhythmias including occurrences of**torsades de pointes*, a potentially fatal arrhythmia. SeeCONTRAINDICATIONSandWARNINGSSections, andPRECAUTIONS: Drug InteractionsSection for specific examples.**
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
Itraconazole Capsules are indicated for the treatment of the following fungal infections in immunocompromised and non-immunocompromisedpatients:
- Blastomycosis, pulmonary and extrapulmonary
- Histoplasmosis, including chronic cavitary pulmonary disease and disseminated, non-meningeal histoplasmosis, and
- Aspergillosis, pulmonary and extrapulmonary, in patients who are intolerant of or who are refractory to amphotericin B therapy.
Specimens for fungal cultures and other relevant laboratory studies (wet mount, histopathology, serology) should be obtained before therapy to isolate and identify causative organisms. Therapy may be instituted before the results of the cultures and other laboratory studies are known; however, once these results become available, antiinfective therapy should be adjusted accordingly.
Itraconazole Capsules are also indicated for the treatment of the following fungal infections in non-immunocompromisedpatients:
- Onychomycosis of the toenail, with or without fingernail involvement, due to dermatophytes (tinea unguium), and
- Onychomycosis of the fingernail due to dermatophytes (tinea unguium).
Prior to initiating treatment, appropriate nail specimens for laboratory testing (KOH preparation, fungal culture, or nail biopsy) should be obtained to confirm the diagnosis of onychomycosis.
(See CLINICAL PHARMACOLOGY: Special Populations, CONTRAINDICATIONS, WARNINGS, and ADVERSE REACTIONS: Post-marketing Experiencefor more information.)
Description of Clinical Studies
Blastomycosis
Analyses were conducted on data from two open-label, non-concurrently controlled studies (N=73 combined) in patients with normal or abnormal immune status. The median dose was 200 mg/day. A response for most signs and symptoms was observed within the first 2 weeks, and all signs and symptoms cleared between 3 and 6 months. Results of these two studies demonstrated substantial evidence of the effectiveness of itraconazole for the treatment of blastomycosis compared with the natural history of untreated cases.
Histoplasmosis
Analyses were conducted on data from two open-label, non-concurrently controlled studies (N=34 combined) in patients with normal or abnormal immune status (not including HIV-infected patients). The median dose was 200 mg/day. A response for most signs and symptoms was observed within the first 2 weeks, and all signs and symptoms cleared between 3 and 12 months. Results of these two studies demonstrated substantial evidence of the effectiveness of itraconazole for the treatment of histoplasmosis, compared with the natural history of untreated cases.
Histoplasmosis in HIV-infected patients
Data from a small number of HIV-infected patients suggested that the response rate of histoplasmosis in HIV-infected patients is similar to that of non-HIV- infected patients. The clinical course of histoplasmosis in HIV-infected patients is more severe and usually requires maintenance therapy to prevent relapse.
Aspergillosis
Analyses were conducted on data from an open-label, "single-patient-use" protocol designed to make itraconazole available in the U.S. for patients who either failed or were intolerant of amphotericin B therapy (N=190). The findings were corroborated by two smaller open-label studies (N=31 combined) in the same patient population. Most adult patients were treated with a daily dose of 200 to 400 mg, with a median duration of 3 months. Results of these studies demonstrated substantial evidence of effectiveness of itraconazole as a second-line therapy for the treatment of aspergillosis compared with the natural history of the disease in patients who either failed or were intolerant of amphotericin B therapy.
Onychomycosis of the toenail
Analyses were conducted on data from three double-blind, placebo-controlled studies (N=214 total; 110 given Itraconazole Capsules) in which patients with onychomycosis of the toenails received 200 mg of Itraconazole Capsules once daily for 12 consecutive weeks. Results of these studies demonstrated mycologic cure, defined as simultaneous occurrence of negative KOH plus negative culture, in 54% of patients. Thirty-five percent (35%) of patients were considered an overall success (mycologic cure plus clear or minimal nail involvement with significantly decreased signs) and 14% of patients demonstrated mycologic cure plus clinical cure (clearance of all signs, with or without residual nail deformity). The mean time to overall success was approximately 10 months. Twenty-one percent (21%) of the overall success group had a relapse (worsening of the global score or conversion of KOH or culture from negative to positive).
Onychomycosis of the fingernail
Analyses were conducted on data from a double-blind, placebo-controlled study (N=73 total; 37 given Itraconazole Capsules) in which patients with onychomycosis of the fingernails received a 1-week course (pulse) of 200 mg of Itraconazole Capsules b.i.d., followed by a 3-week period without Itraconazole Capsules, which was followed by a second 1-week pulse of 200 mg of Itraconazole Capsules b.i.d. Results demonstrated mycologic cure in 61% of patients. Fifty-six percent (56%) of patients were considered an overall success and 47% of patients demonstrated mycologic cure plus clinical cure. The mean time to overall success was approximately 5 months. None of the patients who achieved overall success relapsed.
CONTRAINDICATIONS SECTION
CONTRAINDICATIONS
Congestive Heart Failure
Itraconazole Capsules should not be administered for the treatment of onychomycosis in patients with evidence of ventricular dysfunction such as congestive heart failure (CHF) or a history of CHF. (See BOXED WARNING, WARNINGS, PRECAUTIONS: Drug Interactions-Calcium Channel Blockers, ADVERSE REACTIONS: Post-marketing Experience, and CLINICAL PHARMACOLOGY: Special Populations.)
Drug Interactions
Coadministration of a number of CYP3A4 substrates are contraindicated with itraconazole. Some examples of drugs for which plasma concentrations increase are: methadone, disopyramide, dofetilide, dronedarone, quinidine, isavuconazole, ergot alkaloids (such as dihydroergotamine, ergometrine (ergonovine), ergotamine, methylergometrine (methylergonovine)), irinotecan, lurasidone, oral midazolam, pimozide, triazolam, felodipine, nisoldipine, ivabradine, ranolazine, eplerenone, cisapride, naloxegol, lomitapide, lovastatin, simvastatin, avanafil, ticagrelor, finerenone, voclosporin. In addition, coadministration with colchicine, fesoterodine and solifenacin is contraindicated in subjects with varying degrees of renal or hepatic impairment, and coadministration with eliglustat is contraindicated in subjects that are poor or intermediate metabolizers of CYP2D6 and in subjects taking strong or moderate CYP2D6 inhibitors. (See PRECAUTIONS: Drug InteractionsSection for specific examples.) This increase in drug concentrations caused by coadministration with itraconazole may increase or prolong both the pharmacologic effects and/or adverse reactions to these drugs. For example, increased plasma concentrations of some of these drugs can lead to QT prolongation and ventricular tachyarrhythmias including occurrences of torsade de pointes, a potentially fatal arrhythmia. Some specific examples are listed in PRECAUTIONS: Drug Interactions.
Coadministration with venetoclax is contraindicated in patients with CLL/SLL during the dose initiation and ramp-up phase of venetoclax due to the potential for an increased risk of tumor lysis syndrome.
Itraconazole should not be administered for the treatment of onychomycosis to pregnant patients or to women contemplating pregnancy.
Itraconazole is contraindicated for patients who have shown hypersensitivity to itraconazole. There is limited information regarding cross-hypersensitivity between itraconazole and other azole antifungal agents. Caution should be used when prescribing itraconazole to patients with hypersensitivity to other azoles.
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Itraconazole has been associated with rare cases of serious hepatotoxicity, including liver failure and death. Some of these cases had neither pre- existing liver disease nor a serious underlying medical condition. If clinical signs or symptoms develop that are consistent with liver disease, treatment should be discontinued and liver function testing performed. The risks and benefits of itraconazole use should be reassessed. (See WARNINGS: Hepatic Effectsand PRECAUTIONS: Hepatotoxicityand Information for Patients.)
Adverse Events in the Treatment of Systemic Fungal Infections
Adverse event data were derived from 602 patients treated for systemic fungal disease in U.S. clinical trials who were immunocompromised or receiving multiple concomitant medications. Treatment was discontinued in 10.5% of patients due to adverse events. The median duration before discontinuation of therapy was 81 days (range: 2 to 776 days). The table lists adverse events reported by at least 1% of patients.
Table 3: Clinical Trials of Systemic Fungal Infections: Adverse Events Occurring with an Incidence of Greater than or Equal to 1%|
Body System/Adverse Event |
Incidence (%) (N=602) |
|---|---|
| |
|
Gastrointestinal | |
|
Nausea |
11 |
|
Vomiting |
5 |
|
Diarrhea |
3 |
|
Abdominal Pain |
2 |
|
Anorexia |
1 |
|
Body as a Whole | |
|
Edema |
4 |
|
Fatigue |
3 |
|
Fever |
3 |
|
Malaise |
1 |
|
Skin and Appendages | |
|
Rash * |
9 |
|
Pruritus |
3 |
|
Central/Peripheral Nervous System | |
|
Headache |
4 |
|
Dizziness |
2 |
|
Psychiatric | |
|
Libido Decreased |
1 |
|
Somnolence |
1 |
|
Cardiovascular | |
|
Hypertension |
3 |
|
Metabolic/Nutritional | |
|
Hypokalemia |
2 |
|
Urinary System | |
|
Albuminuria |
1 |
|
Liver and Biliary System | |
|
Hepatic Function Abnormal |
3 |
|
Reproductive System, Male | |
|
Impotence |
1 |
Adverse events infrequently reported in all studies included constipation, gastritis, depression, insomnia, tinnitus, menstrual disorder, adrenal insufficiency, gynecomastia, and male breast pain.
Adverse Events Reported in Toenail Onychomycosis Clinical Trials
Patients in these trials were on a continuous dosing regimen of 200 mg once daily for 12 consecutive weeks.
The following adverse events led to temporary or permanent discontinuation of therapy.
Table 4: Clinical Trials of Onychomycosis of the Toenail: Adverse Events Leading to Temporary or Permanent Discontinuation of Therapy|
Adverse Event |
Incidence (%) |
|---|---|
|
Elevated Liver Enzymes (greater than twice the upper limit of normal) |
4 |
|
Gastrointestinal Disorders |
4 |
|
Rash |
3 |
|
Hypertension |
2 |
|
Orthostatic Hypotension |
1 |
|
Headache |
1 |
|
Malaise |
1 |
|
Myalgia |
1 |
|
Vasculitis |
1 |
|
Vertigo |
1 |
The following adverse events occurred with an incidence of greater than or equal to 1% (N=112): headache: 10%; rhinitis: 9%; upper respiratory tract infection: 8%; sinusitis, injury: 7%; diarrhea, dyspepsia, flatulence, abdominal pain, dizziness, rash: 4%; cystitis, urinary tract infection, liver function abnormality, myalgia, nausea: 3%; appetite increased, constipation, gastritis, gastroenteritis, pharyngitis, asthenia, fever, pain, tremor, herpes zoster, abnormal dreaming: 2%.
Adverse Events Reported in Fingernail Onychomycosis Clinical Trials
Patients in these trials were on a pulse regimen consisting of two 1-week treatment periods of 200 mg twice daily, separated by a 3-week period without drug.
The following adverse events led to temporary or permanent discontinuation of therapy.
Table 5: Clinical Trials of Onychomycosis of the Fingernail: Adverse Events Leading to Temporary or Permanent Discontinuation of Therapy|
Adverse Event |
Incidence (%) |
|---|---|
|
Rash/Pruritus |
3 |
|
Hypertriglyceridemia |
3 |
The following adverse events occurred with an incidence of greater than or equal to 1% (N=37): headache: 8%; pruritus, nausea, rhinitis: 5%; rash, bursitis, anxiety, depression, constipation, abdominal pain, dyspepsia, ulcerative stomatitis, gingivitis, hypertriglyceridemia, sinusitis, fatigue, malaise, pain, injury: 3%.
Adverse Events Reported from Other Clinical Trials
In addition, the following adverse drug reaction was reported in patients who participated in Itraconazole Capsules clinical trials: Hepatobiliary Disorders:hyperbilirubinemia.
The following is a list of additional adverse drug reactions associated with itraconazole that have been reported in clinical trials of SPORANOX ®Oral Solution and itraconazole IV excluding the adverse reaction term "Injection site inflammation" which is specific to the injection route of administration:
Cardiac Disorders:cardiac failure, left ventricular failure, tachycardia;
General Disorders and Administration Site Conditions:face edema, chest pain, chills;
Hepatobiliary Disorders:hepatic failure, jaundice;
Investigations:alanine aminotransferase increased, aspartate aminotransferase increased, blood alkaline phosphatase increased, blood lactate dehydrogenase increased, blood urea increased, gamma-glutamyltransferase increased, urine analysis abnormal;
Metabolism and Nutrition Disorders:hyperglycemia, hyperkalemia, hypomagnesemia;
Psychiatric Disorders:confusional state;
Renal and Urinary Disorders:renal impairment;
Respiratory, Thoracic and Mediastinal Disorders:dysphonia, cough;
Skin and Subcutaneous Tissue Disorders:rash erythematous, hyperhidrosis;
Vascular Disorders:hypotension
Post-marketing Experience
Adverse drug reactions that have been first identified during post-marketing experience with itraconazole (all formulations) are listed in the table below. Because these reactions are reported voluntarily from a population of uncertain size, reliably estimating their frequency or establishing a causal relationship to drug exposure is not always possible.
Table 6: Post-marketing Reports of Adverse Drug Reactions|
Blood and Lymphatic System Disorders: |
Leukopenia, neutropenia, thrombocytopenia |
|
Immune System Disorders: |
Anaphylaxis; anaphylactic, anaphylactoid and allergic reactions; serum sickness; angioneurotic edema |
|
Nervous System Disorders: |
Peripheral neuropathy, paresthesia, hypoesthesia, tremor |
|
Eye Disorders: |
Visual disturbances, including vision blurred and diplopia |
|
Ear and Labyrinth Disorders: |
Transient or permanent hearing loss |
|
Cardiac Disorders: |
Congestive heart failure |
|
Respiratory, Thoracic and Mediastinal Disorders: |
Pulmonary edema, dyspnea |
|
Gastrointestinal Disorders: |
Pancreatitis, dysgeusia |
|
Hepatobiliary Disorders: |
Serious hepatotoxicity (including some cases of fatal acute liver failure), hepatitis |
|
Skin and Subcutaneous Tissue Disorders: |
Toxic epidermal necrolysis, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, erythema multiforme, exfoliative dermatitis, leukocytoclastic vasculitis, alopecia, photosensitivity, urticaria |
|
Musculoskeletal and Connective Tissue Disorders: |
Arthralgia |
|
Renal and Urinary Disorders: |
Urinary incontinence, pollakiuria |
|
Reproductive System and Breast Disorders: |
Erectile dysfunction |
|
General Disorders and Administration Site Conditions: |
Peripheral edema |
|
Investigations: |
Blood creatine phosphokinase increased |
There is limited information on the use of itraconazole during pregnancy. Cases of congenital abnormalities including skeletal, genitourinary tract, cardiovascular and ophthalmic malformations as well as chromosomal and multiple malformations have been reported during post-marketing experience. A causal relationship with itraconazole has not been established. (See CLINICAL PHARMACOLOGY: Special Populations, CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS: Drug Interactionsfor more information.)
SPL UNCLASSIFIED SECTION
For more information call 1-800-667-8570.
Revised: 02/2024
Manufactured for:
Patriot Pharmaceuticals, LLC
Horsham, PA 19044, USA
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
Pharmacokinetics and Metabolism
General Pharmacokinetic Characteristics
Peak plasma concentrations of itraconazole are reached within 2 to 5 hours following oral administration. As a consequence of non-linear pharmacokinetics, itraconazole accumulates in plasma during multiple dosing. Steady-state concentrations are generally reached within about 15 days, with C maxvalues of 0.5 μg/mL, 1.1 μg/mL and 2.0 μg/mL after oral administration of 100 mg once daily, 200 mg once daily and 200 mg b.i.d., respectively. The terminal half-life of itraconazole generally ranges from 16 to 28 hours after single dose and increases to 34 to 42 hours with repeated dosing. Once treatment is stopped, itraconazole plasma concentrations decrease to an almost undetectable concentration within 7 to 14 days, depending on the dose and duration of treatment. Itraconazole mean total plasma clearance following intravenous administration is 278 mL/min. Itraconazole clearance decreases at higher doses due to saturable hepatic metabolism.
Absorption
Itraconazole is rapidly absorbed after oral administration. Peak plasma concentrations of itraconazole are reached within 2 to 5 hours following an oral capsule dose. The observed absolute oral bioavailability of itraconazole is about 55%.
The oral bioavailability of itraconazole is maximal when Itraconazole Capsules are taken immediately after a full meal.
Absorption of itraconazole capsules is reduced in subjects with reduced gastric acidity, such as subjects taking medications known as gastric acid secretion suppressors (e.g., H 2-receptor antagonists, proton pump inhibitors) or subjects with achlorhydria caused by certain diseases. (See PRECAUTIONS: Drug Interactions.) Absorption of itraconazole under fasted conditions in these subjects is increased when Itraconazole Capsules are administered with an acidic beverage (such as a non-diet cola). When Itraconazole Capsules were administered as a single 200-mg dose under fasted conditions with non-diet cola after ranitidine pretreatment, a H 2-receptor antagonist, itraconazole absorption was comparable to that observed when Itraconazole Capsules were administered alone. (See PRECAUTIONS: Drug Interactions.)
Itraconazole exposure is lower with the Capsule formulation than with the Oral Solution when the same dose of drug is given. (See WARNINGS)
Distribution
Most of the itraconazole in plasma is bound to protein (99.8%), with albumin being the main binding component (99.6% for the hydroxy-metabolite). It has also a marked affinity for lipids. Only 0.2% of the itraconazole in plasma is present as free drug. Itraconazole is distributed in a large apparent volume in the body (>700 L), suggesting extensive distribution into tissues. Concentrations in lung, kidney, liver, bone, stomach, spleen and muscle were found to be two to three times higher than corresponding concentrations in plasma, and the uptake into keratinous tissues, skin in particular, up to four times higher. Concentrations in the cerebrospinal fluid are much lower than in plasma.
Metabolism
Itraconazole is extensively metabolized by the liver into a large number of metabolites. In vitrostudies have shown that CYP3A4 is the major enzyme involved in the metabolism of itraconazole. The main metabolite is hydroxy- itraconazole, which has in vitroantifungal activity comparable to itraconazole; trough plasma concentrations of this metabolite are about twice those of itraconazole.
Excretion
Itraconazole is excreted mainly as inactive metabolites in urine (35%) and in feces (54%) within one week of an oral solution dose. Renal excretion of itraconazole and the active metabolite hydroxy-itraconazole account for less than 1% of an intravenous dose. Based on an oral radiolabeled dose, fecal excretion of unchanged drug ranges from 3% to 18% of the dose.
As re-distribution of itraconazole from keratinous tissues appears to be negligible, elimination of itraconazole from these tissues is related to epidermal regeneration. Contrary to plasma, the concentration in skin persists for 2 to 4 weeks after discontinuation of a 4-week treatment and in nail keratin – where itraconazole can be detected as early as 1 week after start of treatment – for at least six months after the end of a 3-month treatment period.
Special Populations
Renal Impairment
Limited data are available on the use of oral itraconazole in patients with renal impairment. A pharmacokinetic study using a single 200 mg oral dose of itraconazole was conducted in three groups of patients with renal impairment (uremia: n=7; hemodialysis: n=7; and continuous ambulatory peritoneal dialysis: n=5). In uremic subjects with a mean creatinine clearance of 13 mL/min. × 1.73 m 2, the exposure, based on AUC, was slightly reduced compared with normal population parameters. This study did not demonstrate any significant effect of hemodialysis or continuous ambulatory peritoneal dialysis on the pharmacokinetics of itraconazole (T max, C max, and AUC 0–8h). Plasma concentration-versus-time profiles showed wide intersubject variation in all three groups. After a single intravenous dose, the mean terminal half- lives of itraconazole in patients with mild (defined in this study as CrCl 50–79 mL/min), moderate (defined in this study as CrCl 20–49 mL/min), and severe renal impairment (defined in this study as CrCl <20 mL/min) were similar to that in healthy subjects (range of means 42–49 hours vs 48 hours in renally impaired patients and healthy subjects, respectively). Overall exposure to itraconazole, based on AUC, was decreased in patients with moderate and severe renal impairment by approximately 30% and 40%, respectively, as compared with subjects with normal renal function. Data are not available in renally impaired patients during long-term use of itraconazole. Dialysis has no effect on the half-life or clearance of itraconazole or hydroxy-itraconazole. (See PRECAUTIONSand DOSAGE AND ADMINISTRATION.)
Hepatic Impairment
Itraconazole is predominantly metabolized in the liver. A pharmacokinetic study was conducted in 6 healthy and 12 cirrhotic subjects who were administered a single 100 mg dose of itraconazole as capsule. A statistically significant reduction in mean C max(47%) and a twofold increase in the elimination half-life (37±17 hours vs. 16±5 hours) of itraconazole were noted in cirrhotic subjects compared with healthy subjects. However, overall exposure to itraconazole, based on AUC, was similar in cirrhotic patients and in healthy subjects. Data are not available in cirrhotic patients during long- term use of itraconazole. (See CONTRAINDICATIONS, PRECAUTIONS: Drug Interactionsand DOSAGE AND ADMINISTRATION.)
Decreased Cardiac Contractility
When itraconazole was administered intravenously to anesthetized dogs, a dose- related negative inotropic effect was documented. In a healthy volunteer study of itraconazole intravenous infusion, transient, asymptomatic decreases in left ventricular ejection fraction were observed using gated SPECT imaging; these resolved before the next infusion, 12 hours later. If signs or symptoms of congestive heart failure appear during administration of Itraconazole Capsules, itraconazole should be discontinued. (See BOXED WARNING, CONTRAINDICATIONS, WARNINGS, PRECAUTIONS: Drug Interactionsand ADVERSE REACTIONS: Post-marketing Experiencefor more information.)
MICROBIOLOGY
Mechanism of Action
In vitrostudies have demonstrated that itraconazole inhibits the cytochrome P450-dependent synthesis of ergosterol, which is a vital component of fungal cell membranes.
Antimicrobial Activity
Itraconazole exhibits in vitroactivity against Blastomyces dermatitidis, Histoplasma capsulatum, Histoplasma duboisii, Aspergillus flavus, Aspergillus fumigatus, and Trichophytonspecies (See INDICATIONS AND USAGE: Description of Clinical Studies).
Susceptibility Testing Methods
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
Resistance
Isolates from several fungal species with decreased susceptibility to itraconazole have been isolated in vitroand from patients receiving prolonged therapy.
Itraconazole is not active against Zygomycetes(e.g., Rhizopusspp., Rhizomucorspp., Mucorspp. and Absidiaspp.), Fusariumspp., Scedosporiumspp. and Scopulariopsisspp.
Cross-Resistance
Several in vitrostudies have reported that some fungal clinical isolates with reduced susceptibility to one azole antifungal agent may also be less susceptible to other azole derivatives. The finding of cross-resistance is dependent on a number of factors, including the species evaluated, its clinical history, the particular azole compounds compared, and the type of susceptibility test that is performed.
Studies (both in vitroand in vivo) suggest that the activity of amphotericin B may be suppressed by prior azole antifungal therapy. As with other azoles, itraconazole inhibits the 14C-demethylation step in the synthesis of ergosterol, a cell wall component of fungi. Ergosterol is the active site for amphotericin B. In one study the antifungal activity of amphotericin B against Aspergillus fumigatusinfections in mice was inhibited by ketoconazole therapy. The clinical significance of test results obtained in this study is unknown.
WARNINGS SECTION
WARNINGS
Hepatic Effects
Itraconazole has been associated with rare cases of serious hepatotoxicity, including liver failure and death. Some of these cases had neither pre- existing liver disease nor a serious underlying medical condition, and some of these cases developed within the first week of treatment. If clinical signs or symptoms develop that are consistent with liver disease, treatment should be discontinued and liver function testing performed. Continued itraconazole use or reinstitution of treatment with itraconazole is strongly discouraged unless there is a serious or life-threatening situation where the expected benefit exceeds the risk. (SeePRECAUTIONS: Information for Patientsand ADVERSE REACTIONS.)
Cardiac Dysrhythmias
Life-threatening cardiac dysrhythmias and/or sudden death have occurred in patients using drugs such as cisapride, pimozide, methadone, or quinidine concomitantly with itraconazole and/or other CYP3A4 inhibitors. Concomitant administration of these drugs with itraconazole is contraindicated. (See BOXED WARNING, CONTRAINDICATIONS, and PRECAUTIONS: Drug Interactions.)
Cardiac Disease
**Itraconazole Capsules should not be administered for the treatment of onychomycosis in patients with evidence of ventricular dysfunction such as congestive heart failure (CHF) or a history of CHF.**Itraconazole Capsules should not be used for other indications in patients with evidence of ventricular dysfunction unless the benefit clearly outweighs the risk.
For patients with risk factors for congestive heart failure, physicians should carefully review the risks and benefits of itraconazole therapy. These risk factors include cardiac disease such as ischemic and valvular disease; significant pulmonary disease such as chronic obstructive pulmonary disease; and renal failure and other edematous disorders. Such patients should be informed of the signs and symptoms of CHF, should be treated with caution, and should be monitored for signs and symptoms of CHF during treatment. If signs or symptoms of CHF appear during administration of Itraconazole Capsules, discontinue administration.
Itraconazole has been shown to have a negative inotropic effect. When itraconazole was administered intravenously to anesthetized dogs, a dose- related negative inotropic effect was documented. In a healthy volunteer study of itraconazole intravenous infusion, transient, asymptomatic decreases in left ventricular ejection fraction were observed using gated SPECT imaging; these resolved before the next infusion, 12 hours later.
Itraconazole has been associated with reports of congestive heart failure. In post-marketing experience, heart failure was more frequently reported in patients receiving a total daily dose of 400 mg although there were also cases reported among those receiving lower total daily doses.
Calcium channel blockers can have negative inotropic effects which may be additive to those of itraconazole. In addition, itraconazole can inhibit the metabolism of calcium channel blockers. Therefore, caution should be used when co-administering itraconazole and calcium channel blockers due to an increased risk of CHF. Concomitant administration of itraconazole and felodipine or nisoldipine is contraindicated.
Cases of CHF, peripheral edema, and pulmonary edema have been reported in the post-marketing period among patients being treated for onychomycosis and/or systemic fungal infections. (See CLINICAL PHARMACOLOGY: Special Populations, CONTRAINDICATIONS, PRECAUTIONS: Drug Interactions, and ADVERSE REACTIONS: Post-marketing Experiencefor more information.)
Interaction Potential
Itraconazole has a potential for clinically important drug interactions. Coadministration of specific drugs with itraconazole may result in changes in efficacy of itraconazole and/or the coadministered drug, life-threatening effects and/or sudden death. Drugs that are contraindicated, not recommended or recommended for use with caution in combination with itraconazole are listed in PRECAUTIONS: Drug Interactions.
Interchangeability
Itraconazole Capsules and SPORANOX ®(itraconazole) Oral Solution should not be used interchangeably. This is because drug exposure is greater with the Oral Solution than with the Capsules when the same dose of drug is given. In addition, the topical effects of mucosal exposure may be different between the two formulations. Only the Oral Solution has been demonstrated effective for oral and/or esophageal candidiasis.
OVERDOSAGE SECTION
OVERDOSAGE
Itraconazole is not removed by dialysis. In the event of accidental overdosage, supportive measures should be employed. Contact a certified poison control center for the most up to date information on the management of Itraconazole Capsules overdosage (1-800-222-1222 or www.poison.org).
In general, adverse events reported with overdose have been consistent with adverse drug reactions already listed in this package insert for itraconazole. (See ADVERSE REACTIONS.)
SPL PATIENT PACKAGE INSERT SECTION
|
This Patient Information has been approved by the U.S. Food and Drug Administration |
Revised: 10/2023 | |||
|
PATIENT INFORMATION | ||||
|
Read this Patient Information that comes with ITRACONAZOLE CAPSULES before you start taking it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. | ||||
|
What is the most important information I should know about ITRACONAZOLE CAPSULES? ITRACONAZOLE CAPSULES can cause serious side effects, including: ***Heart failure.**Do not take ITRACONAZOLE CAPSULES if you have had heart failure, including congestive heart failure. | ||||
|
| |||
|
***Heart problems and other serious medical problems.**Serious medical problems that affect the heart and other parts of your body can happen if you take ITRACONAZOLE CAPSULES with certain other medicines.Do not take ITRACONAZOLE CAPSULES if you also take the following medicines: | ||||
|
|
| ||
|
Do nottake ITRACONAZOLE CAPSULES with venetoclax for chronic lymphocytic leukemia/small lymphocytic lymphoma when you first start treatment with venetoclax or with increasing doses of venetoclax. This is not a complete list of medicines that can interact with ITRACONAZOLE CAPSULES. ITRACONAZOLE CAPSULES may affect the way other medicines work, and other medicines may affect how ITRACONAZOLE CAPSULES works. You can ask your pharmacist for a list of medicines that interact with ITRACONAZOLE CAPSULES. Before you start taking ITRACONAZOLE CAPSULES, tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Before you start any new medicine, ask your healthcare provider or pharmacist if it is safe to take it with ITRACONAZOLE CAPSULES. | ||||
|
*Liver problems. ITRACONAZOLE CAPSULES can cause serious liver problems which may be severe and lead to death.Stop taking ITRACONAZOLE CAPSULES and call your healthcare provider right away if you have any of these symptoms of liver problems: | ||||
|
| |||
|
For more information about side effects, see "What are the possible side effects of ITRACONAZOLE CAPSULES?" | ||||
|
What are ITRACONAZOLE CAPSULES?
| ||||
|
Do not take ITRACONAZOLE CAPSULES if you:
| ||||
|
Before taking ITRACONAZOLE CAPSULES, tell your healthcare provider about all of your medical conditions, including if you:
Taking ITRACONAZOLE CAPSULES with certain medicines may affect each other. Taking ITRACONAZOLE CAPSULES with other medicines can cause serious side effects. | ||||
|
How should I take ITRACONAZOLE CAPSULES?
| ||||
|
What should I avoid while taking ITRACONAZOLE CAPSULES? ITRACONAZOLE CAPSULES can cause dizziness and vision problems. Do not drive or operate machinery until you know how ITRACONAZOLE CAPSULES affect you. | ||||
|
What are the possible side effects of ITRACONAZOLE CAPSULES? ITRACONAZOLE CAPSULES may cause serious side effects, including:
The most common side effects of ITRACONAZOLE CAPSULES include: headache, rash, digestive system problems (such as nausea and vomiting), and edema. Additional possible side effects include upset stomach, constipation, fever, inflammation of the pancreas, menstrual disorder, erectile dysfunction, dizziness, muscle pain, painful joints, unpleasant taste, or hair loss. These are not all the possible side effects of ITRACONAZOLE CAPSULES. | ||||
|
How should I store ITRACONAZOLE CAPSULES?
Keep ITRACONAZOLE CAPSULES and all medicines out of the reach of children. | ||||
|
General information about the safe and effective use of ITRACONAZOLE CAPSULES. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use ITRACONAZOLE CAPSULES for a condition for which they were not prescribed. Do not give ITRACONAZOLE CAPSULES to other people, even if they have the same symptoms that you have. It may harm them. You can ask your doctor or pharmacist for information about ITRACONAZOLE CAPSULES that is written for health professionals. | ||||
|
What are the ingredients in ITRACONAZOLE CAPSULES? Active ingredients: itraconazole Inactive ingredients: hard gelatin capsule, hypromellose, polyethylene glycol (PEG) 20,000, titanium dioxide, FD&C Blue No. 1, FD&C Blue No. 2, D&C Red No. 22 and D&C Red No. 28. Manufactured for: Patriot Pharmaceuticals LLC, Horsham, PA 19044, USA | ||||
DESCRIPTION SECTION
DESCRIPTION
Itraconazole is an azole antifungal agent. Itraconazole is a 1:1:1:1 racemic mixture of four diastereomers (two enantiomeric pairs), each possessing three chiral centers. It may be represented by the following structural formula and nomenclature:
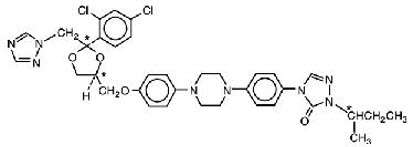
(±)-1-[( R*)- sec-butyl]-4-[ p-[4-[ p-[[(2 R*,4 S*)-2-(2,4-dichlorophenyl)-2-(1 H-1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]-1-piperazinyl]phenyl]-Δ 2-1,2,4-triazolin-5-one mixture with (±)-1-[( R*)- sec-butyl]-4-[ p-[4-[ p-[[(2 S*,4 R*)-2-(2,4-dichlorophenyl)-2-(1 H-1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]-1-piperazinyl]phenyl]-Δ 2-1,2,4-triazolin-5-one
or
(±)-1-[( RS)- sec-butyl]-4-[ p-[4-[ p-[[(2 R,4 S)-2-(2,4-dichlorophenyl)-2-(1 H-1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]-1-piperazinyl]phenyl]-Δ 2-1,2,4-triazolin-5-one
Itraconazole has a molecular formula of C 35H 38Cl 2N 8O 4and a molecular weight of 705.64. It is a white to slightly yellowish powder. It is insoluble in water, very slightly soluble in alcohols, and freely soluble in dichloromethane. It has a pKa of 3.70 (based on extrapolation of values obtained from methanolic solutions) and a log (n-octanol/water) partition coefficient of 5.66 at pH 8.1.
Itraconazole Capsules contain 100 mg of itraconazole coated on sugar spheres (composed of sucrose, maize starch, and purified water). Inactive ingredients are hard gelatin capsule, hypromellose, polyethylene glycol (PEG) 20,000, titanium dioxide, FD&C Blue No. 1, FD&C Blue No. 2, D&C Red No. 22 and D&C Red No. 28.
Meets USP Dissolution Test 2.
PRECAUTIONS SECTION
PRECAUTIONS
General
Itraconazole Capsules should be administered after a full meal. (See CLINICAL PHARMACOLOGY: Pharmacokinetics and Metabolism).
Under fasted conditions, itraconazole absorption was decreased in the presence of decreased gastric acidity. The absorption of itraconazole may be decreased with the concomitant administration of antacids or gastric acid secretion suppressors. Studies conducted under fasted conditions demonstrated that administration with 8 ounces of a non-diet cola beverage resulted in increased absorption of itraconazole in AIDS patients with relative or absolute achlorhydria. This increase relative to the effects of a full meal is unknown. (See CLINICAL PHARMACOLOGY: Pharmacokinetics and Metabolism).
Hepatotoxicity
Rare cases of serious hepatotoxicity have been observed with itraconazole treatment, including some cases within the first week. It is recommended that liver function monitoring be considered in all patients receiving itraconazole. Treatment should be stopped immediately and liver function testing should be conducted in patients who develop signs and symptoms suggestive of liver dysfunction.
Neuropathy
If neuropathy occurs that may be attributable to Itraconazole Capsules, the treatment should be discontinued.
Immunocompromised Patients
In some immunocompromised patients (e.g., neutropenic, AIDS or organ transplant patients), the oral bioavailability of Itraconazole capsules may be decreased. Therefore, the dose should be adjusted based on the clinical response in these patients.
Cystic Fibrosis
If a cystic fibrosis patient does not respond to Itraconazole Capsules, consideration should be given to switching to alternative therapy. For more information concerning the use of itraconazole in cystic fibrosis patients see the prescribing information for SPORANOX ®Oral Solution.
Hearing Loss
Transient or permanent hearing loss has been reported in patients receiving treatment with itraconazole. Several of these reports included concurrent administration of quinidine which is contraindicated (See BOXED WARNING: Drug Interactions, CONTRAINDICATIONS: Drug Interactionsand PRECAUTIONS: Drug Interactions). The hearing loss usually resolves when treatment is stopped, but can persist in some patients.
Information for Patients
- The topical effects of mucosal exposure may be different between Itraconazole Capsules and SPORANOX ®(itraconazole) Oral Solution. Only the Oral Solution has been demonstrated effective for oral and/or esophageal candidiasis. Itraconazole Capsules should not be used interchangeably with SPORANOX ®(itraconazole) Oral Solution.
- Instruct patients to take Itraconazole Capsules with a full meal. Itraconazole Capsules must be swallowed whole.
- Instruct patients about the signs and symptoms of congestive heart failure, and if these signs or symptoms occur during itraconazole administration, they should discontinue itraconazole and contact their healthcare provider immediately.
- Instruct patients to stop itraconazole treatment immediately and contact their healthcare provider if any signs and symptoms suggestive of liver dysfunction develop. Such signs and symptoms may include unusual fatigue, anorexia, nausea and/or vomiting, jaundice, dark urine, or pale stools.
- Instruct patients to contact their physician before taking any concomitant medications with itraconazole to ensure there are no potential drug interactions.
- Instruct patients that hearing loss can occur with the use of itraconazole. The hearing loss usually resolves when treatment is stopped, but can persist in some patients. Advise patients to discontinue therapy and inform their physicians if any hearing loss symptoms occur.
- Instruct patients that dizziness or blurred/double vision can sometimes occur with itraconazole. Advise patients that if they experience these events, they should not drive or use machines.
Drug Interactions
Effect of Itraconazole Capsules on Other Drugs
Itraconazole and its major metabolite, hydroxy-itraconazole, are potent CYP3A4 inhibitors. Itraconazole is an inhibitor of the drug transporters P-glycoprotein and breast cancer resistance protein (BCRP). Consequently, Itraconazole Capsules has the potential to interact with many concomitant drugs resulting in either increased or sometimes decreased concentrations of the concomitant drugs. Increased concentrations may increase the risk of adverse reactions associated with the concomitant drug which can be severe or life-threatening in some cases (e.g., QT prolongation, Torsade de Pointes, respiratory depression, hepatic adverse reactions, hypersensitivity reactions, myelosuppression, hypotension, seizures, angioedema, atrial fibrillation, bradycardia, priapism). Reduced concentrations of concomitant drugs may reduce their efficacy. Table 1 lists examples of drugs that may have their concentrations affected by itraconazole, but it is not a comprehensive list.
Refer to the approved product labeling to become familiar with the interaction pathways, risk potential, and specific actions to be taken with regards to each concomitant drug prior to initiating therapy with Itraconazole Capsules.
Although many of the clinical drug interactions in Table 1 are based on information with a similar azole antifungal, ketoconazole, these interactions are expected to occur with Itraconazole Capsules.
Table 1: Drug Interactions with Itraconazole Capsules that Affect Concomitant Drug Concentrations|
Examples of Concomitant Drugs Within Class |
Prevention or Management | |
|---|---|---|
| ||
|
Drug Interactions with Itraconazole Capsules that Increase Concomitant Drug Concentrations and May Increase Risk of Adverse Reactions Associated with the Concomitant Drug | ||
|
Alpha Blockers | ||
|
Alfuzosin |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Analgesics | ||
|
Methadone |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Fentanyl |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Alfentanil |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Antiarrhythmics | ||
|
Disopyramide |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Digoxin * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Antibacterials | ||
|
Bedaquiline † |
Concomitant Itraconazole Capsules not recommended for more than 2 weeks at any time during bedaquiline treatment. | |
|
Rifabutin |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. See also Table 2. | |
|
Clarithromycin |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. See also Table 2. | |
|
Trimetrexate |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Anticoagulants and Antiplatelets | ||
|
Ticagrelor |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Apixaban |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Cilostazol |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Anticonvulsants | ||
|
Carbamazepine |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. See also Table 2. | |
|
Antidiabetic Drugs | ||
|
Repaglinide * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Antihelminthics, Antifungals and Antiprotozoals | ||
|
Isavuconazonium |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Praziquantel |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Artemether-lumefantrine |
Monitor for adverse reactions. | |
|
Antimigraine Drugs | ||
|
Ergot alkaloids (e.g., dihydroergotamine, ergotamine) |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Eletriptan |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Antineoplastics | ||
|
Irinotecan |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Venetoclax |
Contraindicated during the dose initiation and ramp-up phase in patients with CLL/SLL. Refer to the venetoclax prescribing information for dosing and safety monitoring instructions. | |
|
Mobocertinib * |
Avoid use during and 2 weeks after Itraconazole Capsules treatment. | |
|
Axitinib |
Ibrutinib |
Avoid use during and 2 weeks after Itraconazole Capsules treatment. |
|
Entrectinib * |
Refer to the entrectinib, pemigatinib and talazoparib prescribing information for dosing instructions if concomitant use cannot be avoided. | |
|
Glasdegib |
Refer to the glasdegib prescribing information for safety monitoring if concomitant use cannot be avoided. | |
|
Bortezomib |
Nintedanib |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. For idelalisib, see also Table 2. |
|
Antipsychotics, Anxiolytics and Hypnotics | ||
|
Alprazolam * |
Midazolam (IV) * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. |
|
Zopiclone * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Lurasidone |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Antivirals | ||
|
Daclatasvir |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. For indinavir, see also Table 2. | |
|
Cobicistat |
Monitor for adverse reactions. See also Table 2. | |
|
Elbasvir/grazoprevir |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Glecaprevir/pibrentasvir |
Monitor for adverse reactions. | |
|
Tenofovir disoproxil fumarate |
Monitor for adverse reactions. | |
|
Beta Blockers | ||
|
Nadolol * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Calcium Channel Blockers | ||
|
Felodipine * |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Diltiazem |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. For diltiazem, see also Table 2. | |
|
Cardiovascular Drugs, Miscellaneous | ||
|
Ivabradine |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Aliskiren * |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. For sildenafil and tadalafil, see also Urologic Drugsbelow. | |
|
Bosentan |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Contraceptives**‡** | ||
|
Dienogest |
Monitor for adverse reactions. | |
|
Diuretics | ||
|
Eplerenone |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Gastrointestinal Drugs | ||
|
Cisapride |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Aprepitant |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Netupitant |
Monitor for adverse reactions. | |
|
Immunosuppressants | ||
|
Voclosporin |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Everolimus |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Budesonide (inhalation) * |
Fluticasone (inhalation) * |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. |
|
Lipid-Lowering Drugs | ||
|
Lomitapide |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Atorvastatin * |
Monitor for drug adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Respiratory Drugs | ||
|
Salmeterol |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
SSRIs, Tricyclics and Related Antidepressants | ||
|
Venlafaxine |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Urologic Drugs | ||
|
Avanafil |
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Fesoterodine |
Patients with moderate to severe renal or hepatic impairment: Contraindicated
during and 2 weeks after Itraconazole Capsules treatment. | |
|
Solifenacin |
Patients with severe renal or moderate to severe hepatic impairment:
Contraindicated during and 2 weeks after Itraconazole Capsules treatment. | |
|
Darifenacin |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Dutasteride |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. For sildenafil and tadalafil, see also Cardiovascular Drugsabove. | |
|
Miscellaneous Drugs and Other Substances | ||
|
Colchicine |
Patients with renal or hepatic impairment:Contraindicated during and 2 weeks
after Itraconazole Capsules treatment. | |
|
Eliglustat |
CYP2D6 EMs §taking a strong or moderate CYP2D6 inhibitor, CYP2D6 IMs §, or
CYP2D6 PMs §: Contraindicated during and 2 weeks after Itraconazole Capsules
treatment. | |
|
Lumacaftor/Ivacaftor |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. | |
|
Alitretinoin (oral) |
Monitor for adverse reactions. Concomitant drug dose reduction may be necessary. | |
|
Valbenazine |
Concomitant drug dose reduction is necessary. | |
|
Vasopressin Receptor Antagonists | ||
|
Conivaptan |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Drug Interactions with Itraconazole Capsules that Decrease Concomitant Drug Concentrations and May Reduce Efficacy of the Concomitant Drug | ||
|
Antineoplastics | ||
|
Regorafenib |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Gastrointestinal Drugs | ||
|
Saccharomyces boulardii |
Not recommended during and 2 weeks after Itraconazole Capsules treatment. | |
|
Nonsteroidal Anti-Inflammatory Drugs | ||
|
Meloxicam * |
Concomitant drug dose increase may be necessary. |
Effect of Other Drugs on Itraconazole Capsules
Itraconazole is mainly metabolized through CYP3A4. Other substances that either share this metabolic pathway or modify CYP3A4 activity may influence the pharmacokinetics of itraconazole. Some concomitant drugs have the potential to interact with Itraconazole Capsules resulting in either increased or sometimes decreased concentrations of Itraconazole Capsules. Increased concentrations may increase the risk of adverse reactions associated with Itraconazole Capsules. Decreased concentrations may reduce Itraconazole Capsules efficacy.
Table 2 lists examples of drugs that may affect itraconazole concentrations, but is not a comprehensive list. Refer to the approved product labeling to become familiar with the interaction pathways, risk potential and specific actions to be taken with regards to each concomitant drug prior to initiating therapy with Itraconazole Capsules.
Although many of the clinical drug interactions in Table 2 are based on information with a similar azole antifungal, ketoconazole, these interactions are expected to occur with Itraconazole Capsules.
Table 2: Drug Interactions with Other Drugs that Affect Itraconazole Capsules Concentrations|
Examples of Concomitant Drugs Within Class |
Prevention or Management |
|---|---|
| |
|
Drug Interactions with Other Drugs that Increase Itraconazole Capsules Concentrations and May Increase Risk of Adverse Reactions Associated with Itraconazole Capsules | |
|
Antibacterials | |
|
Ciprofloxacin * |
Monitor for adverse reactions. Itraconazole Capsules dose reduction may be necessary. |
|
Antineoplastics | |
|
Idelalisib |
Monitor for adverse reactions. Itraconazole Capsules dose reduction may be necessary. See also Table 1. |
|
Antivirals | |
|
Cobicistat |
Monitor for adverse reactions. Itraconazole Capsules dose reduction may be necessary. For, cobicistat, elvitegravir, indinavir, ombitasvir/ paritaprevir/ ritonavir with or without dasabuvir, ritonavir, and saquinavir, see also Table 1. |
|
Calcium Channel Blockers | |
|
Diltiazem |
Monitor for adverse reactions. Itraconazole Capsules dose reduction may be necessary. See also Table 1. |
|
Drug Interactions with Other Drugs that Decrease Itraconazole Capsules Concentrations and May Reduce Efficacy of Itraconazole Capsules | |
|
Antibacterials | |
|
Isoniazid |
Not recommended 2 weeks before and during Itraconazole Capsules treatment. |
|
Rifabutin * |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. See also Table 1. |
|
Anticonvulsants | |
|
Phenobarbital |
Not recommended 2 weeks before and during Itraconazole Capsules treatment. |
|
Carbamazepine |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. See also Table 1. |
|
Antivirals | |
|
Efavirenz * |
Not recommended 2 weeks before and during Itraconazole Capsules treatment. |
|
Gastrointestinal Drugs | |
|
Drugs that reduce gastric acidity e.g. acid neutralizing medicines such as aluminum hydroxide, or acid secretion suppressors such as H 2- receptor antagonists and proton pump inhibitors. |
Use with caution. Administer acid neutralizing medicines at least 2 hours before or 2 hours after the intake of Itraconazole Capsules. |
|
Miscellaneous Drugs and Other Substances | |
|
Lumacaftor/Ivacaftor |
Not recommended 2 weeks before, during, and 2 weeks after Itraconazole Capsules treatment. |
Pediatric Population
Interaction studies have only been performed in adults.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
Itraconazole showed no evidence of carcinogenicity potential in mice treated orally for 23 months at dosage levels up to 80 mg/kg/day (approximately 1 time the maximum recommended human dose [MRHD] of 400 mg/day based on body surface area comparisons). Male rats treated with 25 mg/kg/day (0.6 times the MRHD based on body surface area comparisons) had a slightly increased incidence of soft tissue sarcoma. These sarcomas may have been a consequence of hypercholesterolemia, which is a response of rats, but not dogs or humans, to chronic itraconazole administration. Female rats treated with 50 mg/kg/day (1.2 times the MRHD based on body surface area comparisons) had an increased incidence of squamous cell carcinoma of the lung (2/50) as compared to the untreated group. Although the occurrence of squamous cell carcinoma in the lung is extremely uncommon in untreated rats, the increase in this study was not statistically significant.
Itraconazole produced no mutagenic effects when assayed in DNA repair test (unscheduled DNA synthesis) in primary rat hepatocytes, in Ames tests with Salmonella typhimurium(6 strains) and Escherichia coli, in the mouse lymphoma gene mutation tests, in a sex-linked recessive lethal mutation ( Drosophila melanogaster) test, in chromosome aberration tests in human lymphocytes, in a cell transformation test with C3H/10T½ C18 mouse embryo fibroblasts cells, in a dominant lethal mutation test in male and female mice, and in micronucleus tests in mice and rats.
Itraconazole did not affect the fertility of male or female rats treated orally with dosage levels of up to 40 mg/kg/day (1 time the MRHD based on body surface area comparisons), even though parental toxicity was present at this dosage level. More severe signs of parental toxicity, including death, were present in the next higher dosage level, 160 mg/kg/day (4 times the MRHD based on body surface area comparisons).
Pregnancy
Teratogenic Effects
Itraconazole was found to cause a dose-related increase in maternal toxicity, embryotoxicity, and teratogenicity in rats at dosage levels of approximately 40–160 mg/kg/day (1–4 times the MRHD based on body surface area comparisons), and in mice at dosage levels of approximately 80 mg/kg/day (1 time the MRHD based on body surface area comparisons). Itraconazole has been shown to cross the placenta in a rat model. In rats, the teratogenicity consisted of major skeletal defects; in mice, it consisted of encephaloceles and/or macroglossia.
There are no studies in pregnant women. Itraconazole should be used for the treatment of systemic fungal infections in pregnancy only if the benefit outweighs the potential risk.
Itraconazole should not be administered for the treatment of onychomycosis to pregnant patients or to women contemplating pregnancy. Itraconazole should not be administered to women of childbearing potential for the treatment of onychomycosis unless they are using effective measures to prevent pregnancy and they begin therapy on the second or third day following the onset of menses. Highly effective contraception should be continued throughout itraconazole therapy and for 2 months following the end of treatment.
During post-marketing experience, cases of congenital abnormalities have been reported. (See ADVERSE REACTIONS: Post-marketing Experience.)
Nursing Mothers
Itraconazole is excreted in human milk; therefore, the expected benefits of itraconazole therapy for the mother should be weighed against the potential risk from exposure of itraconazole to the infant. The U.S. Public Health Service Centers for Disease Control and Prevention advises HIV-infected women not to breast-feed to avoid potential transmission of HIV to uninfected infants.
Pediatric Use
The efficacy and safety of itraconazole have not been established in pediatric patients.
The long-term effects of itraconazole on bone growth in children are unknown. In three toxicology studies using rats, itraconazole induced bone defects at dosage levels as low as 20 mg/kg/day (0.5 times the MRHD of 400 mg based on body surface area comparisons). The induced defects included reduced bone plate activity, thinning of the zona compacta of the large bones, and increased bone fragility. At a dosage level of 80 mg/kg/day (2 times the MRHD based on body surface area comparisons) over 1 year or 160 mg/kg/day (4 times the MRHD based on body surface area comparisons) for 6 months, itraconazole induced small tooth pulp with hypocellular appearance in some rats.
Geriatric Use
Clinical studies of Itraconazole Capsules did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. It is advised to use Itraconazole Capsules in these patients only if it is determined that the potential benefit outweighs the potential risks. In general, it is recommended that the dose selection for an elderly patient should be taken into consideration, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Transient or permanent hearing loss has been reported in elderly patients receiving treatment with itraconazole. Several of these reports included concurrent administration of quinidine which is contraindicated (See BOXED WARNING: Drug Interactions, CONTRAINDICATIONS: Drug Interactionsand PRECAUTIONS: Drug Interactions).
HIV-Infected Patients
Because hypochlorhydria has been reported in HIV-infected individuals, the absorption of itraconazole in these patients may be decreased.
Renal Impairment
Limited data are available on the use of oral itraconazole in patients with renal impairment. The exposure of itraconazole may be lower in some patients with renal impairment. Caution should be exercised when itraconazole is administered in this patient population and dose adjustment may be needed. (See CLINICAL PHARMACOLOGY: Special Populationsand DOSAGE AND ADMINISTRATION.)
Hepatic Impairment
Limited data are available on the use of oral itraconazole in patients with hepatic impairment. Caution should be exercised when this drug is administered in this patient population. It is recommended that patients with impaired hepatic function be carefully monitored when taking itraconazole. It is recommended that the prolonged elimination half-life of itraconazole observed in the single oral dose clinical trial with Itraconazole Capsules in cirrhotic patients be considered when deciding to initiate therapy with other medications metabolized by CYP3A4.
In patients with elevated or abnormal liver enzymes or active liver disease, or who have experienced liver toxicity with other drugs, treatment with itraconazole is strongly discouraged unless there is a serious or life- threatening situation where the expected benefit exceeds the risk. It is recommended that liver function monitoring be done in patients with pre- existing hepatic function abnormalities or those who have experienced liver toxicity with other medications. (See CLINICAL PHARMACOLOGY: Special Populationsand DOSAGE AND ADMINISTRATION.)
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
Itraconazole Capsules should be taken with a full meal to ensure maximal absorption. Itraconazole Capsules must be swallowed whole.
Itraconazole Capsules are a different preparation than SPORANOX ®(itraconazole) Oral Solution and should not be used interchangeably.
Treatment of Blastomycosis and Histoplasmosis
The recommended dose is 200 mg once daily (2 capsules). If there is no obvious improvement, or there is evidence of progressive fungal disease, the dose should be increased in 100-mg increments to a maximum of 400 mg daily. Doses above 200 mg/day should be given in two divided doses.
Treatment of Aspergillosis
A daily dose of 200 to 400 mg is recommended.
Treatment in Life-Threatening Situations
In life-threatening situations, a loading dose should be used.
Although clinical studies did not provide for a loading dose, it is recommended, based on pharmacokinetic data, that a loading dose of 200 mg (2 capsules) three times daily (600 mg/day) be given for the first 3 days of treatment.
Treatment should be continued for a minimum of three months and until clinical parameters and laboratory tests indicate that the active fungal infection has subsided. An inadequate period of treatment may lead to recurrence of active infection.
Itraconazole Capsules and SPORANOX ®(itraconazole) Oral Solution should not be used interchangeably. Only the Oral Solution has been demonstrated effective for oral and/or esophageal candidiasis.
Treatment of Onychomycosis
Toenails with or without fingernail involvement
The recommended dose is 200 mg (2 capsules) once daily for 12 consecutive weeks.
Treatment of Onychomycosis
Fingernails only
The recommended dosing regimen is 2 treatment pulses, each consisting of 200 mg (2 capsules) b.i.d. (400 mg/day) for 1 week. The pulses are separated by a 3-week period without itraconazole.
Use in Patients with Renal Impairment
Limited data are available on the use of oral itraconazole in patients with renal impairment. Caution should be exercised when this drug is administered in this patient population. (See CLINICAL PHARMACOLOGY: Special Populationsand PRECAUTIONS.)
Use in Patients with Hepatic Impairment
Limited data are available on the use of oral itraconazole in patients with hepatic impairment. Caution should be exercised when this drug is administered in this patient population. (See CLINICAL PHARMACOLOGY: Special Populations, WARNINGS, and PRECAUTIONS.)
HOW SUPPLIED SECTION
HOW SUPPLIED
Itraconazole Capsules are available containing 100 mg of itraconazole, with a blue opaque cap and pink transparent body, imprinted with "PP 100." The capsules are supplied in bottles of 30 capsules (NDC 10147-1700-3).
Store at controlled room temperature 15°–25°C (59°–77°F). Protect from light and moisture.
