Piperacillin and Tazobactam
These highlights do not include all the information needed to use PIPERACILLIN and TAZOBACTAM for Injection safely and effectively. See full prescribing information for PIPERACILLIN and TAZOBACTAM for Injection. PIPERACILLIN and TAZOBACTAM for Injection, for intravenous use Initial U.S. Approval: 1993
1aba753c-d0c2-4b35-917a-9143dd4be468
HUMAN PRESCRIPTION DRUG LABEL
Feb 28, 2024
BluePoint Laboratories
DUNS: 985523874
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
PIPERACILLIN and TAZOBACTAM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
PIPERACILLIN and TAZOBACTAM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
PIPERACILLIN and TAZOBACTAM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
Drug Labeling Information
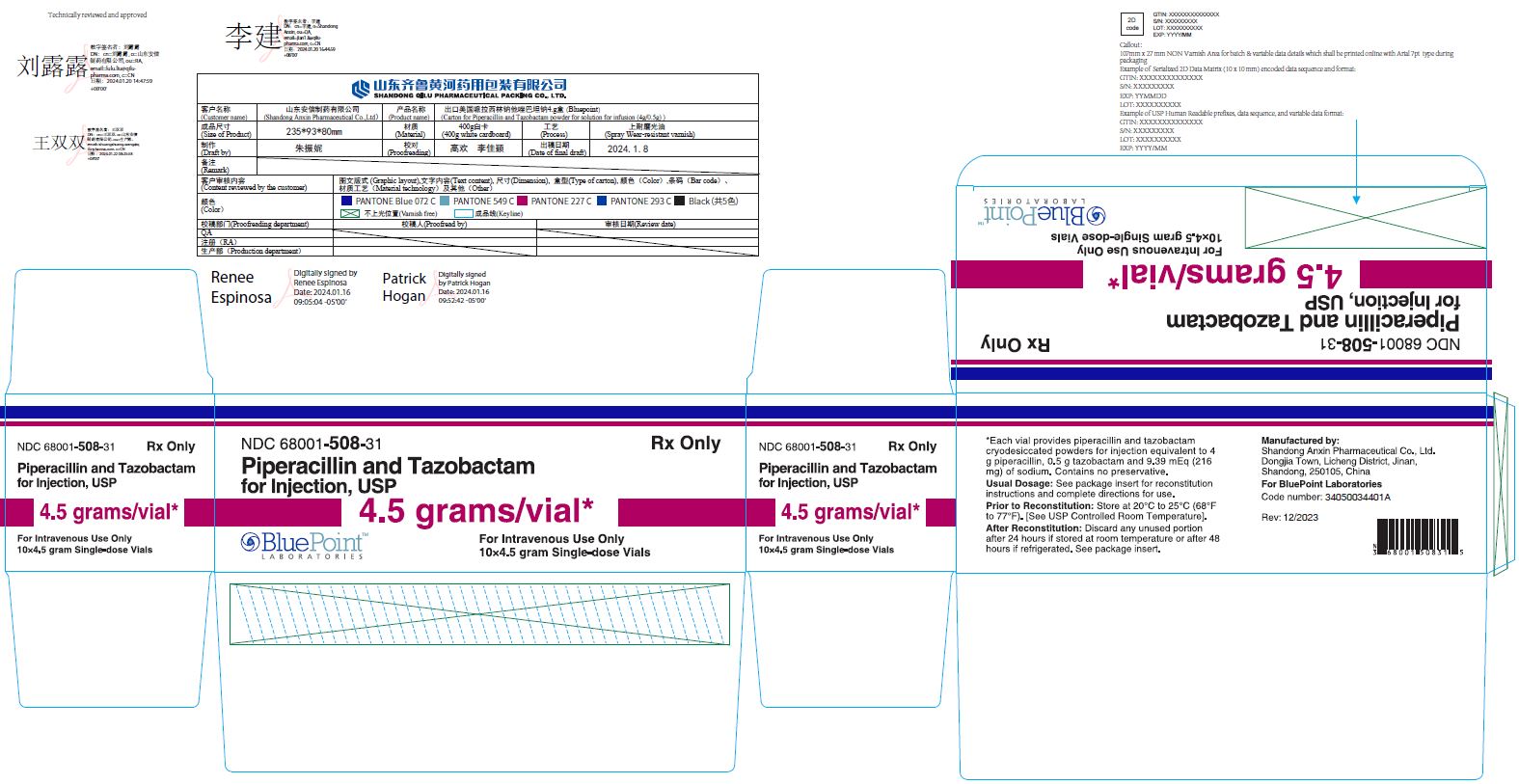
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 4.5 Gram Vial Carton
NDC 68001-508-31
RxOnly
Piperacillin
and Tazobactam
for Injection, USP
4.5 grams/vial*
For Intravenous Use Only
10 x 4.5 gram Single-dose Vials
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Intra-abdominal Infections
Piperacillin and tazobactam for injection, USP is indicated in adults and pediatric patients (2 months of age and older) for the treatment of appendicitis (complicated by rupture or abscess) and peritonitis caused by beta-lactamase producing isolates of Escherichia colior the following members of the Bacteroides fragilisgroup: B. fragilis, B. ovatus, B. thetaiotaomicron, or B. vulgatus.
1.2 Nosocomial Pneumonia
Piperacillin and tazobactam for injection, USP is indicated in adults and pediatric patients (2 months of age and older) for the treatment of nosocomial pneumonia (moderate to severe) caused by beta-lactamase producing isolates of Staphylococcus aureusand by piperacillin and tazobactam-susceptible Acinetobacter baumannii, Haemophilus influenzae, Klebsiella pneumoniae, and Pseudomonas aeruginosa(Nosocomial pneumonia caused by P. aeruginosashould be treated in combination with an aminoglycoside) [seeDosage and Administration (2)] .
1.3 Skin and Skin Structure Infections
Piperacillin and tazobactam for injection, USP is indicated in adults for the treatment of uncomplicated and complicated skin and skin structure infections, including cellulitis, cutaneous abscesses and ischemic/diabetic foot infections caused by beta-lactamase producing isolates of Staphylococcus aureus.
1.4 Female Pelvic Infections
Piperacillin and tazobactam for injection, USP is indicated in adults for the treatment of postpartum endometritis or pelvic inflammatory disease caused by beta-lactamase producing isolates of Escherichia coli.
1.5 Community-acquired Pneumonia
Piperacillin and tazobactam for injection, USP is indicated in adults for the treatment of community-acquired pneumonia (moderate severity only) caused by beta-lactamase producing isolates of Haemophilus influenzae.
1.6 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of piperacillin and tazobactam for injection, USP and other antibacterial drugs, piperacillin and tazobactam for injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Piperacillin and Tazobactam for Injection, USP is a combination of piperacillin, a penicillin-class antibacterial and tazobactam, a beta- lactamase inhibitor, indicated for the treatment of:
- Intra-abdominal infections in adult and pediatric patients 2 months of age and older ( 1.1)
- Nosocomial pneumonia in adult and pediatric patients 2 months of age and older ( 1.2)
- Skin and skin structure infections in adults ( 1.3)
- Female pelvic infections in adults ( 1.4)
- Community-acquired pneumonia in adults ( 1.5)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Piperacillin and Tazobactam for Injection, USP and other antibacterial drugs, piperacillin and tazobactam for injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. ( 1.6)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Piperacillin and tazobactam for injection is contraindicated in patients with a history of allergic reactions to any of the penicillins, cephalosporins, or beta-lactamase inhibitors.
Patients with a history of allergic reactions to any of the penicillins, cephalosporins, or beta-lactamase inhibitors. ( 4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
• Hypersensitivity Adverse Reactions [see Warnings and Precautions ( 5.1)]
• Severe Cutaneous Adverse Reactions [see Warnings and Precautions ( 5.2)]
• Hemophagocytic Lymphohistiocytosis [see Warnings and Precautions ( 5.3)]
• Hematologic Adverse Reactions [see Warnings and Precautions ( 5.4)]
• Central Nervous System Adverse Reactions [see Warnings and Precautions ( 5.5)]
• Nephrotoxicity in Critically Ill Patients [see Warnings and Precautions ( 5.6)]
• Clostridioides difficile-Associated Diarrhea [see Warnings and Precautions ( 5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials in Adult Patients
During the initial clinical investigations, 2621 patients worldwide were treated with piperacillin and tazobactam for injection in phase 3 trials. In the key North American monotherapy clinical trials (n=830 patients), 90% of the adverse events reported were mild to moderate in severity and transient in nature. However, in 3.2% of the patients treated worldwide, piperacillin and tazobactam for injection was discontinued because of adverse events primarily involving the skin (1.3%), including rash and pruritus; the gastrointestinal system (0.9%), including diarrhea, nausea, and vomiting; and allergic reactions (0.5%).
Table 5: Adverse Reactions from Piperacillin and Tazobactam for Injection Monotherapy Clinical Trials|
System Organ Class |
|---|
|
Gastrointestinal disorders |
|
General disorders and administration site conditions |
|
Immune system disorders |
|
Infections and infestations |
|
Metabolism and nutrition disorders |
|
Musculoskeletal and connective tissue disorders |
|
Nervous system disorders |
|
Psychiatric disorders |
|
Skin and subcutaneous tissue disorders |
|
Vascular disorders |
|
Respiratory, thoracic and mediastinal disorders |
Nosocomial Pneumonia Trials
Two trials of nosocomial lower respiratory tract infections were conducted. In one study, 222 patients were treated with piperacillin and tazobactam for injection in a dosing regimen of 4.5 g every 6 hours in combination with an aminoglycoside and 215 patients were treated with imipenem/cilastatin (500 mg/500 mg every 6 hours) in combination with an aminoglycoside. In this trial, treatment-emergent adverse events were reported by 402 patients, 204 (91.9%) in the piperacillin and tazobactam group and 198 (92.1%) in the imipenem/cilastatin group. Twenty-five (11.0 %) patients in the piperacillin and tazobactam group and 14 (6.5%) in the imipenem/cilastatin group (p > 0.05) discontinued treatment due to an adverse event.
The second trial used a dosing regimen of 3.375 g given every 4 hours with an aminoglycoside.
Table 6: Adverse Reactions from Piperacillin and Tazobactam for Injection Plus Aminoglycoside Clinical Trials *|
System Organ Class |
|---|
|
|
Blood and lymphatic system disorders |
|
Gastrointestinal disorders |
|
General disorders and administration site conditions |
|
Infections and infestations |
|
Investigations |
|
Metabolism and nutrition disorders |
|
Nervous system disorders |
|
Psychiatric disorders |
|
Renal and urinary disorders |
|
Skin and subcutaneous tissue disorders |
|
Vascular disorders |
Other Trials: Nephrotoxicity
In a randomized, multicenter, controlled trial in 1200 adult critically ill patients, piperacillin and tazobactam was found to be a risk factor for renal failure (odds ratio 1.7, 95% CI 1.18 to 2.43), and associated with delayed recovery of renal function as compared to other beta-lactam antibacterial drugs. 1[see Warnings and Precautions (5.6)] .
Adverse Laboratory Changes (Seen During Clinical Trials)
Of the trials reported, including that of nosocomial lower respiratory tract infections in which a higher dose of piperacillin and tazobactam for injection was used in combination with an aminoglycoside, changes in laboratory parameters include:
Hematologic—decreases in hemoglobin and hematocrit, thrombocytopenia, increases in platelet count, eosinophilia, leukopenia, neutropenia. These patients were withdrawn from therapy; some had accompanying systemic symptoms (e.g., fever, rigors, chills)
Coagulation—positive direct Coombs' test, prolonged prothrombin time, prolonged partial thromboplastin time
Hepatic—transient elevations of AST (SGOT), ALT (SGPT), alkaline phosphatase, bilirubin
Renal—increases in serum creatinine, blood urea nitrogen
Additional laboratory events include abnormalities in electrolytes (i.e., increases and decreases in sodium, potassium, and calcium), hyperglycemia, decreases in total protein or albumin, blood glucose decreased, gamma- glutamyltransferase increased, hypokalemia, and bleeding time prolonged.
Clinical Trials in Pediatric Patients
Clinical studies of piperacillin and tazobactam for injection in pediatric patients suggest a similar safety profile to that seen in adults.
In a prospective, randomized, comparative, open-label clinical trial of pediatric patients, 2 to 12 years of age, with intra-abdominal infections (including appendicitis and/or peritonitis), 273 patients were treated with piperacillin and tazobactam for injection 112.5 mg/kg given IV every 8 hours and 269 patients were treated with cefotaxime (50 mg/kg) plus metronidazole (7.5 mg/kg) every 8 hours. In this trial, treatment-emergent adverse events were reported by 146 patients, 73 (26.7%) in the piperacillin and tazobactam for injection group and 73 (27.1%) in the cefotaxime/metronidazole group. Six patients (2.2%) in the piperacillin and tazobactam for injection group and 5 patients (1.9%) in the cefotaxime/metronidazole group discontinued due to an adverse event.
In a retrospective, cohort study, 140 pediatric patients 2 months to less than 18 years of age with nosocomial pneumonia were treated with piperacillin and tazobactam for injection and 267 patients were treated with comparators (which included ticarcillin-clavulanate, carbapenems, ceftazidime, cefepime, or ciprofloxacin). The rates of serious adverse reactions were generally similar between the piperacillin and tazobactam for injection and comparator groups, including patients aged 2 months to 9 months treated with piperacillin and tazobactam for injection 90 mg/kg IV every 6 hours and patients older than 9 months and less than 18 years of age treated with piperacillin and tazobactam for injection 112.5 mg/kg IV every 6 hours.
6.2 Postmarketing Experience
In addition to the adverse drug reactions identified in clinical trials in Table 5 and Table 6, the following adverse reactions have been identified during post-approval use of piperacillin and tazobactam for injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hepatobiliary**—**hepatitis, jaundice
Hematologic—hemolytic anemia, agranulocytosis, pancytopenia
Immune—hypersensitivity reactions, anaphylactic/anaphylactoid reactions (including shock), hemophagocytic lymphohistiocytosis (HLH), acute myocardial ischemia with or without myocardial infarction may occur as part of an allergic reaction
Renal**—**interstitial nephritis
Nervous system disorders—seizures
Psychiatric disorders-delirium
Respiratory—eosinophilic pneumonia
Skin and Appendages—erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms, (DRESS), acute generalized exanthematous pustulosis (AGEP), dermatitis exfoliative, and linear IgA bullous dermatosis.
Postmarketing experience with piperacillin and tazobactam for injection in pediatric patients suggests a similar safety profile to that seen in adults.
6.3 Additional Experience with Piperacillin
The following adverse reaction has also been reported for piperacillin for injection:
Skeletal—prolonged muscle relaxation [see Drug Interactions (7.5)] .
The most common adverse reactions (incidence >5%) are diarrhea, constipation, nausea, headache and insomnia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Apotex Corp at 1-800-706-5575 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Aminoglycosides
Piperacillin may inactivate aminoglycosides by converting them to microbiologically inert amides.
In vivoinactivation:
When aminoglycosides are administered in conjunction with piperacillin to patients with end-stage renal disease requiring hemodialysis, the concentrations of the aminoglycosides (especially tobramycin) may be significantly reduced and should be monitored.
Sequential administration of piperacillin and tazobactam for injection and tobramycin to patients with either normal renal function or mild to moderate renal impairment has been shown to modestly decrease serum concentrations of tobramycin but no dosage adjustment is considered necessary.
In vitroinactivation:
Due to the in vitroinactivation of aminoglycosides by piperacillin, piperacillin and tazobactam for injection and aminoglycosides are recommended for separate administration. Piperacillin and tazobactam for injection and aminoglycosides should be reconstituted, diluted, and administered separately when concomitant therapy with aminoglycosides is indicated. Piperacillin and tazobactam for injection is compatible with amikacin and gentamicin for simultaneous Y-site infusion in certain diluents and at specific concentrations. Piperacillin and tazobactam for injection is not compatible with tobramycin for simultaneous Y-site infusion [see Dosage and Administration (2.6)] .
7.2 Probenecid
Probenecid administered concomitantly with piperacillin and tazobactam for injection prolongs the half-life of piperacillin by 21% and that of tazobactam by 71% because probenecid inhibits tubular renal secretion of both piperacillin and tazobactam. Probenecid should not be co-administered with piperacillin and tazobactam for injection unless the benefit outweighs the risk.
7.3 Vancomycin
Studies have detected an increased incidence of acute kidney injury in patients concomitantly administered piperacillin and tazobactam and vancomycin as compared to vancomycin alone [see Warnings and Precautions (5.6)] .
Monitor kidney function in patients concomitantly administered with piperacillin and tazobactam and vancomycin.
No pharmacokinetic interactions have been noted between piperacillin and tazobactam and vancomycin.
7.4 Anticoagulants
Coagulation parameters should be tested more frequently and monitored regularly during simultaneous administration of high doses of heparin, oral anticoagulants, or other drugs that may affect the blood coagulation system or the thrombocyte function [see Warnings and Precautions (5.4)] .
7.5 Vecuronium
Piperacillin when used concomitantly with vecuronium has been implicated in the prolongation of the neuromuscular blockade of vecuronium. Piperacillin and tazobactam for injection could produce the same phenomenon if given along with vecuronium. Due to their similar mechanism of action, it is expected that the neuromuscular blockade produced by any of the non-depolarizing muscle relaxants could be prolonged in the presence of piperacillin. Monitor for adverse reactions related to neuromuscular blockade (see package insert for vecuronium bromide).
7.6 Methotrexate
Limited data suggests that co-administration of methotrexate and piperacillin may reduce the clearance of methotrexate due to competition for renal secretion. The impact of tazobactam on the elimination of methotrexate has not been evaluated. If concurrent therapy is necessary, serum concentrations of methotrexate as well as the signs and symptoms of methotrexate toxicity should be frequently monitored.
7.7 Effects on Laboratory Tests
There have been reports of positive test results using the Bio-Rad Laboratories Platelia Aspergillus EIA test in patients receiving piperacillin and tazobactam injection who were subsequently found to be free of Aspergillus infection. Cross-reactions with non-Aspergillus polysaccharides and polyfuranoses with the Bio-Rad Laboratories Platelia Aspergillus EIA test have been reported. Therefore, positive test results in patients receiving piperacillin and tazobactam should be interpreted cautiously and confirmed by other diagnostic methods.
As with other penicillins, the administration of piperacillin and tazobactam for injection may result in a false-positive reaction for glucose in the urine using a copper-reduction method (CLINITEST ®). It is recommended that glucose tests based on enzymatic glucose oxidase reactions be used.
- Piperacillin and tazobactam for injection administration can significantly reduce tobramycin concentrations in hemodialysis patients. Monitor tobramycin concentrations in these patients.( 7.1)
- Probenecid prolongs the half-lives of piperacillin and tazobactam and should not be co-administered with piperacillin and tazobactam for injection unless the benefit outweighs the risk. ( 7.2)
- Co-administration of piperacillin and tazobactam for injection with vancomycin may increase the incidence of acute kidney injury. Monitor kidney function in patients receiving piperacillin and tazobactam for injection and vancomycin. ( 7.3)
- Monitor coagulation parameters in patients receiving piperacillin and tazobactam for injection and heparin or oral anticoagulants. ( 7.4)
- Piperacillin and tazobactam for injection may prolong the neuromuscular blockade of vecuronium and other non-depolarizing muscle relaxants. Monitor for adverse reactions related to neuromuscular blockade. ( 7.5)
SPL UNCLASSIFIED SECTION
Manufactured by:
Shandong Anxin Pharmaceutical Co., Ltd.
Dongjia Town, Licheng District, Jinan, Shandong, 250105, China
For BluePoint Laboratories
CLINITEST ®is a registered trademark of Siemens Healthcare Diagnostics Inc.
Code number: 34050034311B
Rev: 01/2024
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Piperacillin and tazobactam for injection, USP is a white to off-white powder in vials:
- 2.25 g single-dose vial (piperacillin sodium equivalent to 2 grams of piperacillin and tazobactam sodium equivalent to 0.25 g of tazobactam).
- 3.375 g single-dose vial (piperacillin sodium equivalent to 3 grams of piperacillin and tazobactam sodium equivalent to 0.375 g of tazobactam).
- 4.5 g single-dose vial (piperacillin sodium equivalent to 4 grams of piperacillin and tazobactam sodium equivalent to 0.5 g of tazobactam).
Piperacillin and tazobactam for injection, USP: 2.25 g, 3.375 g, and 4.5 g lyophilized powder for reconstitution in single-dose vials. ( 3, 16)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Piperacillin and tazobactam cross the placenta in humans. However, there are insufficient data with piperacillin and/or tazobactam in pregnant women to inform a drug-associated risk for major birth defects and miscarriage. No fetal structural abnormalities were observed in rats or mice when piperacillin and tazobactam was administered intravenously during organogenesis at doses 1 to 2 times and 2 to 3 times the human dose of piperacillin and tazobactam, respectively, based on body-surface area (mg/m 2). However, fetotoxicity in the presence of maternal toxicity was observed in developmental toxicity and peri/postnatal studies conducted in rats (intraperitoneal administration prior to mating and throughout gestation or from gestation day 17 through lactation day 21) at doses less than the maximum recommended human daily dose based on body-surface area (mg/m 2) [ seeError! Hyperlink reference not valid.].
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
Data
Animal Data
In embryo-fetal development studies in mice and rats, pregnant animals received intravenous doses of piperacillin and tazobactam up to 3000/750 mg/kg/day during the period of organogenesis. There was no evidence of teratogenicity up to the highest dose evaluated, which is 1 to 2 times and 2 to 3 times the human dose of piperacillin and tazobactam, in mice and rats respectively, based on body-surface area (mg/m 2). Fetal body weights were reduced in rats at maternally toxic doses at or above 500/62.5 mg/kg/day, minimally representing 0.4 times the human dose of both piperacillin and tazobactam based on body-surface area (mg/m 2).
A fertility and general reproduction study in rats using intraperitoneal administration of tazobactam or the combination piperacillin and tazobactam prior to mating and through the end of gestation, reported a decrease in litter size in the presence of maternal toxicity at 640 mg/kg/day tazobactam (4 times the human dose of tazobactam based on body-surface area), and decreased litter size and an increase in fetuses with ossification delays and variations of ribs, concurrent with maternal toxicity at ≥640/160 mg/kg/day piperacillin and tazobactam (0.5 times and 1 times the human dose of piperacillin and tazobactam, respectively, based on body-surface area).
Peri/postnatal development in rats was impaired with reduced pup weights, increased stillbirths, and increased pup mortality concurrent with maternal toxicity after intraperitoneal administration of tazobactam alone at doses ≥320 mg/kg/day (2 times the human dose based on body surface area) or of the combination piperacillin and tazobactam at doses ≥640/160 mg/kg/day (0.5 times and 1 times the human dose of piperacillin and tazobactam, respectively, based on body-surface area) from gestation day 17 through lactation day 21.
8.2 Lactation
Risk Summary
Piperacillin is excreted in human milk; tazobactam concentrations in human milk have not been studied. No information is available on the effects of piperacillin and tazobactam on the breast-fed child or on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for piperacillin and tazobactam for injection and any potential adverse effects on the breastfed child from piperacillin and tazobactam for injection or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of piperacillin and tazobactam for injection for intra-abdominal infections, and nosocomial pneumonia have been established in pediatric patients 2 months of age and older.
Use of piperacillin and tazobactam for injection in pediatric patients 2 months of age and older with intra-abdominal infections including appendicitis and/or peritonitis is supported by evidence from well-controlled studies and pharmacokinetic studies in adults and in pediatric patients. This includes a prospective, randomized, comparative, open-label clinical trial with 542 pediatric patients 2 to 12 years of age with intra-abdominal infections (including appendicitis and/or peritonitis), in which 273 pediatric patients received piperacillin and tazobactam. [see Adverse Reactions (6.1)and Clinical Pharmacology (12.3)] .
Use of piperacillin and tazobactam for injection in pediatric patients 2 months of age and older with nosocomial pneumonia is supported by evidence from well-controlled studies in adults with nosocomial pneumonia, a simulation study performed with a population pharmacokinetic model, and a retrospective, cohort study of pediatric patients with nosocomial pneumonia in which 140 pediatric patients were treated with piperacillin and tazobactam for injection and 267 patients treated with comparators (which included ticarcillin- clavulanate, carbapenems, ceftazidime, cefepime, or ciprofloxacin) [see Adverse Reactions (6.1)and Clinical Pharmacology (12.3)].
The safety and effectiveness of piperacillin and tazobactam for injection have not been established in pediatric patients less than 2 months of age [see Clinical Pharmacology (12)and Dosage and Administration (2)] .
Dosage of piperacillin and tazobactam for injection in pediatric patients with renal impairment has not been determined.
8.5 Geriatric Use
Patients over 65 years are not at an increased risk of developing adverse effects solely because of age. However, dosage should be adjusted in the presence of renal impairment [see Dosage and Administration (2)] .
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Piperacillin and tazobactam for injection contains 54 mg (2.35 mEq) of sodium per gram of piperacillin in the combination product. At the usual recommended doses, patients would receive between 648 and 864 mg/day (28.2 and 37.6 mEq) of sodium. The geriatric population may respond with a blunted natriuresis to salt loading. This may be clinically important with regard to such diseases as congestive heart failure.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Renal Impairment
In patients with creatinine clearance ≤ 40 mL/min and dialysis patients (hemodialysis and CAPD), the intravenous dose of piperacillin and tazobactam for injection should be reduced to the degree of renal function impairment [see Dosage and Administration (2)] .
8.7 Hepatic Impairment
Dosage adjustment of piperacillin and tazobactam for injection is not warranted in patients with hepatic cirrhosis [see Clinical Pharmacology (12.3)] .
8.8 Patients with Cystic Fibrosis
As with other semisynthetic penicillins, piperacillin therapy has been associated with an increased incidence of fever and rash in cystic fibrosis patients.
Dosage in patients with renal impairment (creatinine clearance ≤40 mL/min) should be reduced based on the degree of renal impairment. ( 2.3, 8.6)
OVERDOSAGE SECTION
10 OVERDOSAGE
There have been postmarketing reports of overdose with piperacillin and tazobactam. The majority of those events experienced, including nausea, vomiting, and diarrhea, have also been reported with the usual recommended dosages. Patients may experience neuromuscular excitability or seizures if higher than recommended doses are given intravenously (particularly in the presence of renal failure) [see Warnings and Precautions (5.4)] .
Treatment should be supportive and symptomatic according to the patient's clinical presentation. Excessive serum concentrations of either piperacillin or tazobactam may be reduced by hemodialysis. Following a single 3.375 g dose of piperacillin and tazobactam, the percentage of the piperacillin and tazobactam dose removed by hemodialysis was approximately 31% and 39%, respectively [see Clinical Pharmacology (12)] .
DESCRIPTION SECTION
11 DESCRIPTION
Piperacillin and tazobactam for injection, USP is an injectable antibacterial combination products consisting of the semisynthetic antibacterial piperacillin sodium and the beta-lactamase inhibitor tazobactam sodium for intravenous administration.
Piperacillin sodium is derived from D(-)-α-aminobenzyl-penicillin. The chemical name of piperacillin sodium is sodium (2 S,5 R,6 R)-6-[( R)-2-(4-ethyl-2,3-dioxo-1-piperazine-carboxamido)-2- phenylacetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate. The chemical formula is C 23H 26N 5NaO 7S and the molecular weight is 539.5. The chemical structure of piperacillin sodium is:

Tazobactam sodium, a derivative of the penicillin nucleus, is a penicillanic acid sulfone. Its chemical name is sodium (2 S,3 S,5 R)-3-methyl-7-oxo-3-(1 H-1,2,3-triazol-1-ylmethyl)-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate-4,4-dioxide. The chemical formula is C 10H 11N 4NaO 5S and the molecular weight is 322.3. The chemical structure of tazobactam sodium is:

Piperacillin and tazobactam for injection, USP is a white to off-white sterile, cryodesiccated powder consisting of piperacillin and tazobactam as their sodium salts packaged in glass vials. The product does not contain excipients or preservatives.
- Each piperacillin and tazobactam for injection, USP 2.25 g single dose vial contains an amount of drug sufficient for withdrawal of piperacillin sodium equivalent to 2 grams of piperacillin and tazobactam sodium equivalent to 0.25 g of tazobactam. Each vial contains 4.69 mEq (108 mg) of sodium.
- Each piperacillin and tazobactam for injection, USP 3.375 g single dose vial contains an amount of drug sufficient for withdrawal of piperacillin sodium equivalent to 3 grams of piperacillin and tazobactam sodium equivalent to 0.375 g of tazobactam. Each vial contains 7.04 mEq (162 mg) of sodium.
- Each piperacillin and tazobactam for injection, USP 4.5 g single dose vial contains an amount of drug sufficient for withdrawal of piperacillin sodium equivalent to 4 grams of piperacillin and tazobactam sodium equivalent to 0.5 g of tazobactam. Each vial contains 9.39 mEq (216 mg) of sodium.
Piperacillin and tazobactam for injection, USP contains a total of 2.35 mEq (54 mg) of sodium (Na +) per gram of piperacillin in the combination product.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Piperacillin and tazobactam for injection, USP is an antibacterial drug [see Microbiology (12.4)] .
12.2 Pharmacodynamics
The pharmacodynamic parameter for piperacillin and tazobactam that is most predictive of clinical and microbiological efficacy is time above MIC.
12.3 Pharmacokinetics
The mean and coefficients of variation (CV%) for the pharmacokinetic parameters of piperacillin and tazobactam after multiple intravenous doses are summarized in Table 7.
Table 7: Mean (CV%) Piperacillin and Tazobactam PK Parameters|
C max: maximum observed concentration, AUC: Area under the curve,
CL=clearance, CL R= Renal clearance | ||||||
| ||||||
|
Piperacillin | ||||||
|
Piperacillin/Tazobactam Dose * |
C max |
AUC † |
CL |
V |
T 1/2(h) |
CL R |
|
2.25 g |
134 |
131 [14] |
257 |
17.4 |
0.79 |
-- |
|
3.375 g |
242 |
242 [10] |
207 |
15.1 |
0.84 |
140 |
|
4.5 g |
298 |
322 [16] |
210 |
15.4 |
0.84 |
-- |
|
Tazobactam | ||||||
|
Piperacillin/Tazobactam Dose * |
C max |
AUC † |
CL |
V |
T 1/2(h) |
CL R |
|
2.25 g |
15 |
16.0 [21] |
258 |
17.0 |
0.77 |
-- |
|
3.375 g |
24 |
25.0 [8] |
251 |
14.8 |
0.68 |
166 |
|
4.5 g |
34 |
39.8 [15] |
206 |
14.7 |
0.82 |
-- |
Peak plasma concentrations of piperacillin and tazobactam are attained immediately after completion of an intravenous infusion of piperacillin and tazobactam for injection. Piperacillin plasma concentrations, following a 30-minute infusion of piperacillin and tazobactam for injection, were similar to those attained when equivalent doses of piperacillin were administered alone. Steady-state plasma concentrations of piperacillin and tazobactam were similar to those attained after the first dose due to the short half-lives of piperacillin and tazobactam.
Distribution
Both piperacillin and tazobactam are approximately 30% bound to plasma proteins. The protein binding of either piperacillin or tazobactam is unaffected by the presence of the other compound. Protein binding of the tazobactam metabolite is negligible.
Piperacillin and tazobactam are widely distributed into tissues and body fluids including intestinal mucosa, gallbladder, lung, female reproductive tissues (uterus, ovary, and fallopian tube), interstitial fluid, and bile. Mean tissue concentrations are generally 50% to 100% of those in plasma. Distribution of piperacillin and tazobactam into cerebrospinal fluid is low in subjects with non-inflamed meninges, as with other penicillins (see Table 8)
Table 8: Piperacillin/Tazobactam Concentrations in Selected Tissues and Fluids after Single 4 g/0.5 g 30-min IV Infusion of Piperacillin and Tazobactam for Injection|
aEach subject provided a single sample. | ||||||
|
bTime from the start of the infusion | ||||||
|
Tissue or |
N****a |
Sampling |
Mean PIP |
Tissue: |
Tazo |
Tazo Tissue: |
|
Skin |
35 |
0.5 - 4.5 |
34.8 - 94.2 |
0.60 - 1.1 |
4.0 - 7.7 |
0.49 - 0.93 |
|
Fatty Tissue |
37 |
0.5 - 4.5 |
4.0 - 10.1 |
0.097 - 0.115 |
0.7 - 1.5 |
0.10 - 0.13 |
|
Muscle |
36 |
0.5 - 4.5 |
9.4 - 23.3 |
0.29 - 0.18 |
1.4 - 2.7 |
0.18 - 0.30 |
|
Proximal |
7 |
1.5 - 2.5 |
31.4 |
0.55 |
10.3 |
1.15 |
|
Distal |
7 |
1.5 - 2.5 |
31.2 |
0.59 |
14.5 |
2.1 |
|
Appendix |
22 |
0.5 - 2.5 |
26.5 - 64.1 |
0.43 - 0.53 |
9.1 - 18.6 |
0.80 - 1.35 |
Metabolism
Piperacillin is metabolized to a minor microbiologically active desethyl metabolite. Tazobactam is metabolized to a single metabolite that lacks pharmacological and antibacterial activities.
Excretion
Following single or multiple piperacillin and tazobactam for injection doses to healthy subjects, the plasma half-life of piperacillin and of tazobactam ranged from 0.7 to 1.2 hours and was unaffected by dose or duration of infusion.
Both piperacillin and tazobactam are eliminated via the kidney by glomerular filtration and tubular secretion. Piperacillin is excreted rapidly as unchanged drug with 68% of the administered dose excreted in the urine. Tazobactam and its metabolite are eliminated primarily by renal excretion with 80% of the administered dose excreted as unchanged drug and the remainder as the single metabolite. Piperacillin, tazobactam and desethyl piperacillin are also secreted into the bile.
Specific Populations
Renal Impairment
After the administration of single doses of piperacillin and tazobactam to subjects with renal impairment, the half-life of piperacillin and of tazobactam increases with decreasing creatinine clearance. At creatinine clearance below 20 mL/min, the increase in half-life is twofold for piperacillin and fourfold for tazobactam compared to subjects with normal renal function. Dosage adjustments for piperacillin and tazobactam for injection are recommended when creatinine clearance is below 40 mL/min in patients receiving the usual recommended daily dose of piperacillin and tazobactam for injection. See Dosage and Administration (2)for specific recommendations for the treatment of patients with renal - impairment.
Hemodialysis removes 30% to 40% of a piperacillin and tazobactam dose with an additional 5% of the tazobactam dose removed as the tazobactam metabolite. Peritoneal dialysis removes approximately 6% and 21% of the piperacillin and tazobactam doses, respectively, with up to 16% of the tazobactam dose removed as the tazobactam metabolite. For dosage recommendations for patients undergoing hemodialysis [see Dosage and Administration (2)] .
Hepatic Impairment
The half-life of piperacillin and of tazobactam increases by approximately 25% and 18%, respectively, in patients with hepatic cirrhosis compared to healthy subjects. However, this difference does not warrant dosage adjustment of piperacillin and tazobactam for injection due to hepatic cirrhosis.
Pediatrics
Piperacillin and tazobactam pharmacokinetics were studied in pediatric patients 2 months of age and older. The clearance of both compounds is slower in the younger patients compared to older children and adults.
In a population PK analysis, estimated clearance for 9 month-old to 12 year- old patients was comparable to adults, with a population mean (SE) value of 5.64 (0.34) mL/min/kg. The piperacillin clearance estimate is 80% of this value for pediatric patients 2 to 9 months old. In patients younger than 2 months of age, clearance of piperacillin is slower compared to older children; however, it is not adequately characterized for dosing recommendations. The population mean (SE) for piperacillin volume of distribution is 0.243 (0.011) L/kg and is independent of age.
Geriatrics
The impact of age on the pharmacokinetics of piperacillin and tazobactam was evaluated in healthy male subjects, aged 18 to 35 years (n=6) and aged 65 to 80 years (n=12). Mean half-life for piperacillin and tazobactam was 32% and 55% higher, respectively, in the elderly compared to the younger subjects. This difference may be due to age-related changes in creatinine clearance.
Race
The effect of race on piperacillin and tazobactam was evaluated in healthy male volunteers. No difference in piperacillin or tazobactam pharmacokinetics was observed between Asian (n=9) and Caucasian (n=9) healthy volunteers who received single 4/0.5 g doses.
Drug Interactions
The potential for pharmacokinetic drug interactions between piperacillin and tazobactam for injection and aminoglycosides, probenecid, vancomycin, heparin, vecuronium, and methotrexate has been evaluated [see Drug Interactions (7)] .
12.4 Microbiology
Mechanism of Action
Piperacillin sodium exerts bactericidal activity by inhibiting septum formation and cell wall synthesis of susceptible bacteria. In vitro, piperacillin is active against a variety of Gram-positive and Gram-negative aerobic and anaerobic bacteria. Tazobactam sodium has little clinically relevant in vitroactivity against bacteria due to its reduced affinity to penicillin-binding proteins. It is, however, a beta-lactamase inhibitor of the Molecular class A enzymes, including Richmond-Sykes class III (Bush class 2b & 2b') penicillinases and cephalosporinases. It varies in its ability to inhibit class II and IV (2a & 4) penicillinases. Tazobactam does not induce chromosomally-mediated beta-lactamases at tazobactam concentrations achieved with the recommended dosage regimen.
Antimicrobial Activity
Piperacillin and tazobactam for injection has been shown to be active against most isolates of the following microorganisms both in vitroand in clinical infections [see Indications and Usage (1)]:
Aerobic bacteria
Gram-positive bacteria
Staphylococcus aureus(methicillin susceptible isolates only)
Gram-negative bacteria
Acinetobacter baumannii
Escherichia coli
Haemophilus influenzae(excluding beta-lactamase negative, ampicillin-resistant
isolates)
Klebsiella pneumoniae
Pseudomonas aeruginosa(given in combination with an aminoglycoside to which
the isolate is susceptible)
Anaerobic bacteria
Bacteroides fragilisgroup ( B. fragilis, B. ovatus, B. thetaiotaomicron,and B. vulgatus)
The following in vitrodata are available, but their clinical significance is unknown.
At least 90 percent of the following bacteria exhibit an in vitrominimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for piperacillin and tazobactam against isolates of similar genus or organism group.
However, the efficacy of piperacillin and tazobactam for injection in treating clinical infections caused by these bacteria has not been established in adequate and well-controlled clinical trials.
Aerobic bacteria
Gram-positive bacteria
Enterococcus faecalis(ampicillin or penicillin-susceptible isolates only)
Staphylococcus epidermidis(methicillin susceptible isolates only)
Streptococcus agalactiae†
Streptococcus pneumoniae† (penicillin-susceptible isolates only)
Streptococcus pyogenes†
Viridans group streptococci †
Gram-negative bacteria
Citrobacter koseri
Moraxella catarrhalis
Morganella morganii
Neisseria gonorrhoeae
Proteus mirabilis
Proteus vulgaris
Serratia marcescens
Providencia stuartii
Providencia rettgeri
Salmonella enterica
Anaerobic bacteria
Clostridium perfringens
Bacteroides distasonis
Prevotella melaninogenica
†These are not beta-lactamase producing bacteria and, therefore, are susceptible to piperacillin alone.
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
REFERENCES SECTION
15 REFERENCES
- Jensen J-US, Hein L, Lundgren B, et al. BMJ Open 2012; 2:e000635. doi:10.1136.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Piperacillin and tazobactam for injection, USP are supplied as single-dose vials in the following sizes:
- Each piperacillin and tazobactam for injection, USP 2.25 g vial provides piperacillin sodium equivalent to 2 grams of piperacillin and tazobactam sodium equivalent to 0.25 g of tazobactam. Each vial contains 4.69 mEq (108 mg) of sodium. Single dose vial – NDC 68001-506-28, supplied 10 per box - NDC 68001-506-30
- Each piperacillin and tazobactam for injection, USP 3.375 g vial provides piperacillin sodium equivalent to 3 grams of piperacillin and tazobactam sodium equivalent to 0.375 g of tazobactam. Each vial contains 7.04 mEq (162 mg) of sodium. Single dose vial – NDC 68001-507-53, supplied 10 per box - NDC 68001-507-82
- Each piperacillin and tazobactam for injection, USP 4.5 g vial provides piperacillin sodium equivalent to 4 grams of piperacillin and tazobactam sodium equivalent to 0.5 g of tazobactam. Each vial contains 9.39 mEq (216 mg) of sodium. Single dose vial – NDC 68001-508-29, supplied 10 per box - NDC 68001-508-31
Piperacillin and tazobactam for injection, USP vials should be stored at controlled room temperature (20°C to 25°C [68°F to 77°F]) prior to reconstitution.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term carcinogenicity studies in animals have not been conducted with piperacillin and tazobactam, piperacillin, or tazobactam.
Mutagenesis
Piperacillin and tazobactam was negative in microbial mutagenicity assays, the unscheduled DNA synthesis (UDS) test, a mammalian point mutation (Chinese hamster ovary cell HPRT) assay, and a mammalian cell (BALB/c-3T3) transformation assay. In vivo, piperacillin and tazobactam did not induce chromosomal aberrations in rats.
Fertility
Reproduction studies have been performed in rats and have revealed no evidence of impaired fertility when piperacillin and tazobactam is administered intravenously up to a dose of 1280/320 mg/kg piperacillin and tazobactam, which is similar to the maximum recommended human daily dose based on body- surface area (mg/m 2).
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Serious Hypersensitivity Reactions
Advise patients, their families, or caregivers that serious hypersensitivity reactions, including serious allergic cutaneous reactions, could occur with use of piperacillin and tazobactam for injection that require immediate treatment. Ask them about any previous hypersensitivity reactions to piperacillin and tazobactam for injection, other beta-lactams (including cephalosporins), or other allergens [see Warnings and Precautions (5.2)] .
Hemophagocytic Lymphohistiocytosis
Prior to initiation of treatment with piperacillin and tazobactam for injection, inform patients that excessive immune activation may occur with piperacillin and tazobactam for injection and that they should report signs or symptoms such as fever, rash, or lymphadenopathy to a healthcare provider immediately [see Warnings and Precautions ( 5.3)] .
Diarrhea
Advise patients, their families, or caregivers that diarrhea is a common problem caused by antibacterial drugs, including piperacillin and tazobactam for injection, which usually ends when the drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the drug. If this occurs, patients should contact their physician as soon as possible [see Warnings and Precautions (5.8)]
Antibacterial Resistance
Patients should be counseled that antibacterial drugs including piperacillin and tazobactam for injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When piperacillin and tazobactam for injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by piperacillin and tazobactam for injection or other antibacterial drugs in the future.
Pregnancy and Lactation
Patients should be counseled that piperacillin and tazobactam for injection can cross the
placenta in humans and is excreted in human milk [see Use in Specific Population (8.1, 8.2)]
