TRANYLCYPROMINE SULFATE
These highlights do not include all the information needed to use TRANYLCYPROMINE SULFATE TABLETS safely and effectively. See full prescribing information for TRANYLCYPROMINE SULFATE TABLETS.TRANYLCYPROMINE SULFATE USP tablets, for oral useInitial U.S. Approval: 1961
7974d4ad-c419-4c7f-bbd6-f631d53e30de
HUMAN PRESCRIPTION DRUG LABEL
May 26, 2023
Strides Pharma Science Limited
DUNS: 650738743
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
tranylcypromine sulfate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
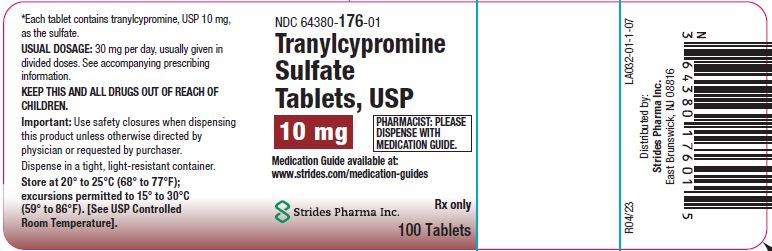
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 64380-176-01
Tranylcypromine Sulfate Tablets, USP
10 mg
Medication Guide available at: www.strides.com/medication-guides
Rx only
Strides Pharma Inc.
100 Tablets
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
4.1 Combination with Certain Drugs
Concomitant use of tranylcypromine sulfate or use in rapid succession with the products inTable 1 is contraindicated. Such use may cause severe or life- threatening reactions such as hypertensive crises or serotonin syndrome [see Drug Interactions (7.1)]. Medication-free periods between administration of tranylcypromine sulfate and contraindicated agents are recommended [see Dosage and Administration (2.2) and Drug Interactions (7.1)].
Table 1: Products Contraindicated with the Use of Tranylcypromine Sulfate|
** Drug Classes** | ||
|
Non-selective H1 receptor antagonists | ||
|
Antidepressants including but not limited to:
| ||
|
Amphetamines and methylphenidates and derivatives | ||
|
Sympathomimetic products (e.g., cold, hay fever or weight-reducing products that contain vasoconstrictors such as pseudoephedrine, phenylephrine, and ephedrine; or dietary supplements that contain sympathomimetics) | ||
|
Triptans | ||
|
** Individual Drugs (not included in the above classes)** | ||
|
buspirone |
levodopa |
s-adenosyl-L-methionine (SAM-e) |
|
carbamazepine |
meperidine |
tapentadol |
|
cyclobenzaprine |
methyldopa |
tetrabenazine |
|
dextromethorphan |
milnacipran |
tryptophan |
|
dopamine |
rasagiline | |
|
hydroxytryptophan |
reserpine |
4.2 Pheochromocytoma and Catecholamine-Releasing Paragangliomas
Tranylcypromine Sulfate is contraindicated in the presence of pheochromocytoma or other catecholamine-releasing paragangliomas because such tumors secrete pressor substances and can lead to hypertensive crisis [see Warnings and Precautions (5.3)].
- Concomitant use or use in rapid succession with other MAOIs; selective serotonin reuptake inhibitors; serotonin and norepinephrine reuptake inhibitors; tricyclic antidepressants; sympathomimetic drugs; and numerous other drugs. See Full Prescribing Information for the full list of contraindicated products (4.1, 7.1)
- Pheochromocytoma, other catecholamine-releasing paraganglioma (4.2)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behaviors in Adolescents and Young Adults
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients and 4,500 pediatric patients, the incidence of suicidal thoughts and behaviors in antidepressant-treated patients age 24 years and younger was greater than in placebo-treated patients. There was considerable variation in risk of suicidal thoughts and behaviors among drugs, but there was an increased risk identified in young patients for most drugs studied. There were differences in absolute risk of suicidal thoughts and behaviors across the different indications, with the highest incidence in patients with MDD. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1000 patients treated are provided inTable 2.
Table 2: Risk Differences of the Number of Patients of Suicidal Thoughts and Behavior in the Pooled Placebo-Controlled Trials of Antidepressants in Pediatric and Adult Patients|
** Age Range** |
** Drug-Placebo Difference in Number of Patients of Suicidal Thoughts or Behaviors per 1000 Patients Treated** |
|
** Increases Compared to Placebo** | |
|
<18 years old |
14 additional patients |
|
18 to 24 years old |
5 additional patients |
|
** Decreases Compared to Placebo** | |
|
25 to 64 years old |
1 fewer patient |
|
≥65 years old |
6 fewer patients |
It is unknown whether the risk of suicidal thoughts and behaviors in children, adolescents, and young adults extends to longer-term use, i.e., beyond four months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with MDD that antidepressants delay the recurrence of depression and that depression itself is a risk factor for suicidal thoughts and behaviors.
Monitor all antidepressant-treated patients for any indication for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy, and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing tranylcypromine sulfate, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
5.2 Hypertensive Crisis and Hypertension
Hypertensive Crisis
MAOIs, including tranylcypromine sulfate, have been associated with hypertensive crises caused by the ingestion of foods or beverages with a high concentration of tyramine. In addition, hypertensive reactions and crises may occur with concomitant use of other drugs [see Drug Interactions (7.1)]. Patients with hyperthyroidism may be at greater risk of hypertensive crisis
Signs, Symptoms, and Complications of Hypertensive Crisis: In some patients a hypertensive crisis constitutes a hypertensive emergency, which requires immediate attention to prevent serious complications or fatal outcome. These emergencies are characterized by severe hypertension (e.g., with a blood pressure of more than 180/120 mm Hg) and evidence of organ dysfunction. Symptoms may include occipital headache (which may radiate frontally), palpitations, neck stiffness or soreness, nausea or vomiting, sweating (sometimes with fever or cold, clammy skin), dilated pupils, photophobia, shortness of breath, or confusion. Either tachycardia or bradycardia may be present and may be associated with constricting chest pain. Seizures may also occur. Intracranial bleeding, sometimes fatal, has been reported in association with the increase in blood pressure.
Strategies to Reduce the Risk of Hypertensive Crisis: Instruct patients to avoid foods and beverages with high tyramine content while being treated with tranylcypromine sulfate and for 2 weeks after stopping tranylcypromine sulfate [see Drug Interactions (7.2)]. Careful evaluation of the benefits and risks of tranylcypromine sulfate therapy is necessary in patients with:
- Hypertension or confirmed or suspected cerebrovascular or cardiovascular disorders that constitute an increased risk for complications from severe hypertension, and
- A history of headaches that can mask the occurrence of headaches as prodromal of a hypertensive crisis.
In all patients taking tranylcypromine sulfate, monitor blood pressure closely to detect evidence of increased blood pressure. Full reliance should not be placed on blood pressure readings. The patient should also be observed for other signs and symptoms of hypertensive crisis.
Treatment of Hypertensive Crisis: Therapy should be interrupted with symptoms that may be prodromal or a manifestation of a hypertensive crisis, such as palpitations or headaches, and patients should be evaluated immediately. Discontinue tranylcypromine sulfate, other drugs, foods or beverages suspected to contribute to the hypertensive crisis immediately [see Drug Interactions (7.1, 7.2)].
Patients with severe elevations in blood pressure (e.g., more than 180/120 mm Hg) with evidence of organ dysfunction require immediate blood pressure reduction. Fever should be managed by means of external cooling. However, additional measures to control the causes of hyperthermia (psychomotor agitation, increased neuromuscular activity, persistent seizures) may be required.
Hypertension
Clinically significant increases in blood pressure have also been reported after the administration of MAOIs, including tranylcypromine sulfate, in patients not ingesting tyramine-rich foods or beverages. Assess blood pressure before prescribing tranylcypromine sulfate and closely monitor blood pressure in all patients taking tranylcypromine sulfate.
5.3 Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with MAOIs when used concomitantly with other serotonergic drugs. Such drugs include SSRIs, SNRIs, tricyclic antidepressants, triptans, fentanyl, lithium, tramadol, tryptophan, buspirone, St. John's wort, S-adenosyl-L-methionine (SAM-e), and other MAOIs used to treat nonpsychiatric disorders (such as linezolid or intravenous methylene blue).
Manifestations of the serotonin syndrome may include mental status changes (e.g., agitation, hallucinations, delirium, coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia; with possible rapid fluctuations of vital signs), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyper-reflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Fatal outcome of serotonin syndrome has been reported, including in patients who had been treated with tranylcypromine sulfate. In some cases of an interaction between tranylcypromine sulfate and SSRIs or SNRIs, the features of the syndrome resembled neuroleptic malignant syndrome.
The concomitant use, or use in rapid succession, of tranylcypromine sulfate with other serotonergic drugs is contraindicated. However, there may be circumstances when treatment with other serotonergic substances (such as linezolid or intravenous methylene blue) is necessary and cannot be delayed. In such cases, tranylcypromine sulfate must be discontinued as soon as possible before initiating treatment with the other agent.
Treatment with tranylcypromine sulfate and any concomitant serotonergic agents should be discontinued immediately if the above events occur, and supportive symptomatic treatment should be initiated.
5.4 Activation of Mania/Hypomania
In patients with bipolar disorder, treating a depressive episode with tranylcypromine sulfate or another antidepressant may precipitate a mixed/manic episode. Prior to initiating treatment with tranylcypromine sulfate, screen patients for any personal or family history of bipolar disorder, mania, or hypomania.
5.5 Hypotension
Hypotension, including postural hypotension, has been observed during therapy with Tranylcypromine Sulfate. At doses above 30 mg daily, postural hypotension is a major adverse reaction and may result in syncope. Symptoms of postural hypotension are seen most commonly, but not exclusively, in patients with pre- existing hypertension. Blood pressure usually returns rapidly to pretreatment levels upon discontinuation of tranylcypromine sulfate.
Dosage increases should be made more gradually in patients with a tendency toward hypotension and/or postural hypotension (e.g., elderly patients) [see Dosage and Administration (2.2) and Use in Specific Populations (8.5)]. Such patients should be closely observed for postural changes in blood pressure throughout treatment. Also, when tranylcypromine sulfate is used concomitantly with other agents known to cause hypotension, the possibility of additive hypotensive effects should be considered [see Drug Interactions (7.1)]. Postural hypotension may be relieved by having patients lie down until blood pressure returns to normal.
5.6 Hypotension and Hypertension during Anesthesia and Perioperative Care
It is recommended that tranylcypromine sulfate be discontinued at least 10 days prior to elective surgery. If this is not possible, for general anesthesia, regional and local anesthesia, and perioperative care avoid the use of agents that are contraindicated for concomitant use with tranylcypromine sulfate. Carefully consider the risk of agents and techniques that increase the risk for hypotension (e.g., epidural or spinal anesthesia) or other adverse reactions to tranylcypromine sulfate (e.g., hypertension associated with the use of vasoconstrictors in local anesthetics).
5.7 Need for Emergency Treatment with Contraindicated Drugs
If in the absence of therapeutic alternatives emergency treatment with a contraindicated product (e.g., linezolid, intravenous methylene blue, direct- acting sympathomimetic drugs such as epinephrine) becomes necessary and cannot be delayed, discontinue tranylcypromine sulfate as soon as possible before initiating treatment with the other product and monitor closely for adverse reactions [see Drug Interactions (7.1)].
5.8 Discontinuation Syndrome
Abrupt discontinuation or dosage reduction of tranylcypromine sulfate has been associated with the appearance of new symptoms that include dizziness, nausea, headache, irritability, insomnia, diarrhea, anxiety, fatigue, abnormal dreams, and hyperhidrosis. In general, discontinuation events occurred more frequently with longer duration of therapy.
There have been spontaneous reports of adverse reactions occurring upon discontinuation of MAOIs, particularly when abrupt, including dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g. paresthesia, such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. While these reactions are generally self-limiting, there have been reports of prolonged discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with tranylcypromine sulfate. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible [see Dosage and Administration (2.3) and Adverse Reactions (6)].
5.9 Risk of Clinically Significant Adverse Reactions due to Persistence of
MAO Inhibition after Discontinuation
Although excretion of tranylcypromine sulfate is rapid, inhibition of MAO may persist up to 10 days following discontinuation. This should be taken into account when considering the use of potentially interacting substances or the consumption of tyramine-rich food or beverages [see Drug Interactions (7.4)], or when interpreting adverse reactions observed after discontinuation of tranylcypromine sulfate. Care should be taken to differentiate symptoms of persistent MAO inhibition from withdrawal symptoms [see Drug Abuse and Dependence (9.3)].
5.10 Hepatotoxicity
Hepatitis and elevated aminotransferases have been reported in association with tranylcypromine sulfate administration. Patients should be monitored accordingly. Tranylcypromine Sulfate should be discontinued in patients who develop signs and symptoms of hepatotoxicity.
Sedation has occurred in tranylcypromine sulfate-treated patients with cirrhosis. Patients with cirrhosis receiving tranylcypromine sulfate should be monitored for possible increased risks of central nervous system adverse reactions, such as excessive drowsiness.
5.11 Seizures
Seizures have been reported with tranylcypromine sulfate withdrawal after abuse, and with overdose. Patients at risk for seizures should be monitored accordingly.
5.12 Hypoglycemia in Diabetic Patients
Some MAOIs have contributed to hypoglycemic episodes in diabetic patients receiving insulin or other blood-glucose-lowering agents. Monitor blood glucose in patients receiving both tranylcypromine sulfate and blood-glucose- lowering agents. A reduction of the dosage of such agents may be necessary [see Drug Interactions (7.1)]
5.13 Aggravation of Coexisting Symptoms of Depression
Tranylcypromine sulfate may aggravate coexisting symptoms in depression, such as anxiety and agitation.
5.14 Adverse Effects on the Ability to Drive and Operate Machinery
Some tranylcypromine sulfate adverse reactions (e.g., hypotension, faintness, drowsiness, confusion, disorientation) can impair a patient's ability to operate machinery or use an automobile. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that tranylcypromine sulfate therapy does not impair their ability to engage in such activities.
- Activation of Mania/Hypomania : May be precipitated by antidepressant treatment in patients with bipolar disorder. Screen patients prior to treatment (5.4)
- Hypotension (including syncope) : Monitor patients and adjust tranylcypromine sulfate dosage or concomitant medication as necessary (5.5)
- Hypotension and Hypertension during Anesthesia and Perioperative Care : If possible, discontinue tranylcypromine sulfate prior to elective surgery (5.6)
- Hepatitis and Elevated Liver Enzymes : Monitor accordingly (5.10)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Clinically Significant Drug Interactions
Tables 3 and 4 lists drug classes and individual products, respectively, with a potential for interaction with tranylcypromine sulfate, describes the predominant observed or anticipated risks, and provides advice on concomitant use. Given serious adverse reactions with multiple agents, patients should avoid taking over-the-counter medications or dietary supplements without prior consultation with a healthcare provider able to provide advice on the potential for interactions.
Time to Start Tranylcypromine Sulfate after Discontinuation of a Contraindicated Drug
For products that are contraindicated with tranylcypromine sulfate, a time period of 4 to 5 half-lives of the other product or any active metabolite should elapse before starting treatment with tranylcypromine sulfate. After stopping treatment with an MAO inhibitor antidepressant, a time period of at least 1 week or 4 to 5 half-lives of the other MAO inhibitor (whichever is longer) should elapse before starting treatment with tranylcypromine sulfate because of the risk for clinically significant adverse reactions after discontinuation due to persistent MAO inhibition [see Dosage and Administration (2.2), Warnings and Precautions (5.9)]. This period can be several weeks long (e.g., a minimum of 5 weeks for fluoxetine given fluoxetine's long half-life). Refer to the prescribing information of the contraindicated product for relevant information.
Time to Start Contraindicated Drug after Discontinuation of Tranylcypromine Sulfate
The potential for interactions persists after discontinuation of tranylcypromine sulfate until MAO activity has sufficiently recovered. Inhibition of MAO may persist up to 10 days following discontinuation [see Warnings and Precautions (5.9)]. After stopping tranylcypromine sulfate, at least 1 week should elapse before starting another MAOI (intended to treat MDD) or other contraindicated antidepressants. Refer to the prescribing information of any agent considered for subsequent use for recommendations on the duration of a waiting period after discontinuation of a MAO inhibitor.
If in the absence of therapeutic alternatives and emergency treatment with a contraindicated drug (e.g., linezolid, intravenous methylene blue, direct- acting sympathomimetic drugs such as epinephrine) becomes necessary and cannot be delayed, discontinue tranylcypromine sulfate as soon as possible before initiating treatment with the other agent, and monitor closely for adverse reactions.
Table 3 Clinically Significant Drug Interactions with Drug Classes*
| ||
|
** Sympathomimetic drugs include amphetamines as well as cold, hay fever or weight-reducing products that contain vasoconstrictors such as pseudoephedrine, phenylephrine, and ephedrine) | ||
|
a[See Contraindications (4.1)] ; b[See Warnings and Precautions (5.2)] ; c[See Warnings and Precautions (5.3)] | ||
|
d If not otherwise specified in this table, consider avoiding concomitant use (see also information on medication-free intervals, use agent at the lowest appropriate dosage, monitor for effects of the interaction, advise the patient to report potential effects). | ||
|
e [See Warnings and Precautions (5.5)] ; f [See Warnings and Precautions (5.14)] ; g[See Overdosage (10.1)] | ||
|
** Product** |
** Clinical Comment on Concomitant Use****a** |
** Predominant Effect/Risk [Hypertensive Reaction (HR)bor Serotonin Syndrome (SS)c]** |
|
Agents with blood pressure-reducing effects |
Use with cautiond |
Hypotensione |
|
Non-selective H1 receptor antagonists |
Contraindicateda |
Increased anticholinergic effects |
|
Beta-adrenergic blockers (see also agents or procedures with blood pressure- reducing effects) |
Use with the cautiond |
More pronounced bradycardia, postural hypotensione |
|
Blood glucose-lowering agents |
Dosage reduction of such agents may be necessary. Monitor blood glucose. |
Excessive reduction of blood glucose (additive effect)f |
|
CNS depressant agents (including opioids, alcohol, sedatives, hypnotics) |
Use with cautiond |
Increased CNS depression |
|
Dietary supplements containing sympathomimetics |
Contraindicateda | |
|
Antidepressants including but not limited to:
|
Contraindicateda |
SS for all antidepressants |
|
Amphetamines and methylphenidates and derivatives |
Contraindicateda |
HR |
|
Sympathomimetic drugs** |
Contraindicateda |
HR; Including risk of intracerebral hemorrhage |
|
Triptans |
Contraindicateda |
SS |
|
*Some drugs in this table may also belong to groups listed in Table 3 above, and may be associated with additional interactions. | ||
|
a[See Contraindications (4.1)] ; b[See Warnings and Precautions (5.3)] ; c[See Warnings and Precautions (5.7)] dIf not otherwise specified in this table, consider avoiding concomitant use (see also information on medication-free intervals , use agent at the lowest appropriate dose, monitor for effects of the interaction, advise the patient to report potential effects, and be prepared to discontinue the agent and treat effects of the interaction | ||
|
e[See Warnings and Precautions (5.5)] | ||
|
** Product** |
** Clinical Comment on Concomitant Use****a** |
** Predominant Effect/Risk**** [Hypertensive Reaction (HR)bor Serotonin Syndrome (SS)c]** |
|
Altretamine |
Use with cautiond |
Orthostatic hypotensione |
|
Buspirone |
Contraindicateda |
HR |
|
Carbamazepine |
Contraindicateda |
SS |
|
Chlorpromazine |
Use with cautiond |
Hypotensive effectse |
|
Cyclobenzaprine |
Contraindicateda |
SS |
|
Dextromethorphan |
Contraindicateda |
SS; Psychosis, bizarre behavior |
|
Dopamine |
Contraindicateda |
HR |
|
Droperidol |
Use with cautiond |
QT interval prolongation |
|
Entacapone |
Use with cautiond |
HR |
|
Fentanyl |
Use with cautiond |
SS |
|
Hydroxytryptophan |
Contraindicateda |
SS |
|
Levodopa |
Contraindicateda |
HR |
|
Lithium |
Use with cautiond |
SS |
|
Meperidine |
Contraindicateda |
SS |
|
Methadone |
Use with cautiond |
SS |
|
Methyldopa |
Contraindicateda |
HR |
|
Metoclopramide |
Use with cautiond |
HR/SS |
|
Mirtazapine |
Contraindicateda |
SS |
|
Oxcarbazepine |
Use with cautiond because of close structural relationship with tricyclic antidepressants |
SS |
|
Rasagiline |
Contraindicateda |
HR |
|
Reserpine |
Contraindicateda |
HR |
|
S-adenosyl-L-methionine (SAM-e) |
Contraindicateda |
SS |
|
Tapentadol |
Contraindicateda |
HR/SS |
|
Tetrabenazine |
Contraindicateda |
HR |
|
Tolcapone |
Use with cautiond |
HR |
|
Tramadol |
Use with cautiond |
SS; Increased seizure risk |
|
Tryptophan |
Contraindicateda |
SS |
7.2 Tyramine-Containing Foods and Beverages
Tranylcypromine Sulfate inhibits intestinal MAO, which is responsible for the catabolism of tyramine in food and beverages. As a result of this inhibition, large amounts of tyramine may enter the systemic circulation and precipitate a sudden elevation in blood pressure or hypertensive crisis [see Warnings and Precautions (5.2)]. Instruct tranylcypromine sulfate-treated patients to avoid foods and beverages with significant tyramine content during treatment with tranylcypromine sulfate or within 2 weeks of stopping treatment (seeTable 5 for a list of food and beverages containing significant amounts of tyramine).
Table 5: Foods and Beverages with and without Significant Amounts of Tyramine|
** Class of Food or** |
** Tyramine-Rich Foods and** |
** Acceptable Foods and Drinks, Containing No or Little Tyramine** |
|
Meat, Poultry, and Fish |
Air dried, aged and fermented meats, sausages and salamis (including cacciatore, hard salami and mortadella); pickled herring; and any spoiled or improperly stored meat, poultry, and fish (e.g., foods that have undergone changes in coloration, odo, or become moldy); spoiled or improperly stored animal livers |
Fresh meat, poultry, and fish, including fresh processed meats (e.g., lunch meats, hot dogs, breakfast sausage, and cooked sliced ham) |
|
Vegetables |
Broad bean pods (fava bean pods) |
All other vegetables |
|
Dairy |
Aged cheeses |
Processed cheeses, mozzarella, ricotta cheese, cottage cheese, and yogurt |
|
Beverages |
All varieties of tap beer and beers that have not been pasteurized so as to allow for ongoing fermentation and excessive amounts of caffeine. |
Concomitant use of alcohol with tranylcypromine sulfate is not recommended. (Bottled and canned beers and wines contain little or no tyramine.) |
|
Other |
Concentrated yeast extract (e.g., Marmite), sauerkraut, most soybean products (including soy sauce and tofu), OTC supplements containing tyramine, and chocolate |
Brewer's yeast, baker's yeast, soy milk, commercial chain restaurant pizzas prepared with cheeses low in tyramine |
See Full Prescribing Information for a list of products, foods and beverages that can interact with tranylcypromine sulfate (7) (7)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Tranylcypromine Sulfate Tablets, USP are for oral use. The recommended dosage is 30 mg per day (in divided doses). If patients do not have an adequate response, increase the dosage in increments of 10 mg per day every 1 to 3 weeks to a maximum 30 mg twice daily (60 mg per day). Dosage increases should be made more gradually in patients at risk for hypotension (e.g., geriatric patients) [see Warnings and Precautions (5.5)].
2.2 Switching to or from Other Antidepressants
Switching from Contraindicated Antidepressants to Tranylcypromine Sulfate
After stopping treatment with contraindicated antidepressants, a time period of 4 to 5 half-lives of the other antidepressant or any active metabolite should elapse before starting treatment with tranylcypromine sulfate. After stopping treatment with an MAO inhibitor antidepressant, a time period of at least one week or 4 to 5 half-lives of the other MAO inhibitor (whichever is longer) should elapse before starting treatment with tranylcypromine sulfate to reduce the risk of additive effects [see Contraindications (4.1) and Drug Interactions (7.1)].
Switching from Tranylcypromine Sulfate to Other MAOIs or Contraindicated Antidepressants
After stopping tranylcypromine sulfate treatment, at least one week should elapse before starting another MAOI (intended to treat MDD) or other contraindicated antidepressants. Refer to the prescribing information of the subsequently used drug for product-specific advice on a medication-free interval [see Contraindications (4.1) and Drug Interactions (7.1)].
2.3 Discontinuing Treatment
Withdrawal effects, including delirium, have been reported with abrupt discontinuation of tranylcypromine sulfate therapy. Higher daily doses and longer duration of use appear to be associated with a higher risk of withdrawal effects. Consider discontinuing tranylcypromine sulfate therapy by slow, gradual dosage reduction [see Warnings and Precautions (5.8) and Drug Abuse and Dependence (9.3)].
2.4 Screen for Bipolar Disorder and Elevated Blood Pressure Prior to
Starting Tranylcypromine Sulfate
Prior to initiating treatment with tranylcypromine sulfate:
- Screen patients for a history of mania [see Warnings and Precautions (5.4)].
- Measure blood pressure [see Warnings and Precautions (5.2, 5.5)].
- Recommended daily dosage is 30 mg in divided doses (2.1)
- If no adequate response, increase dosage in increments of 10 mg per day every 1 to 3 weeks to a maximum dosage of 30 mg twice daily (60 mg per day). Consider more gradual dosage increases in patients at risk for hypotension (2.1)
- Consider discontinuing tranylcypromine sulfate therapy gradually because of the risk for withdrawal effects (2.3, 5.8, 9.3)
- Switching from or to other MAOIs or other antidepressants: See full prescribing information for instructions (2.2, 7.1)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are limited published reports of placental infarction and congenital anomalies in association with use of tranylcypromine sulfate during pregnancy; however, these reports may not adequately inform the presence or absence of drug-associated risk with the use of tranylcypromine sulfate during pregnancy. In the U.S. general population, the background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Animal embryo-fetal development studies were not conducted with tranylcypromine; however, published animal reproduction studies report placental transfer of tranylcypromine in rats and a dose-dependent decrease in uterine blood flow in pregnant sheep. Advise pregnant women of the potential risk to a fetus.
Clinical Considerations
Labor or Delivery
During labor and delivery, the potential for interactions between tranylcypromine sulfate and drugs or procedures (e.g., epidural anesthesia) should be taken into account in women who have received tranylcypromine sulfate [see Warnings and Precautions (5.6) and Drug Interactions (7.1)].
8.2 Lactation
Risk Summary
Tranylcypromine is present in human milk. There is no available information on the effects of tranylcypromine on milk production. There is no available information on the effects of tranylcypromine on a breastfed child; however, because of the potential for serious adverse reactions in a breastfed infant, advise nursing women to discontinue breastfeeding during treatment with tranylcypromine sulfate.
8.4 Pediatric Use
Safety and effectiveness of tranylcypromine sulfate in the pediatric population have not been established. All risks associated with the use of tranylcypromine sulfate, including the risk of suicidal thoughts and behavior, apply to adults and pediatric patients [see Boxed Warning and Warnings and Precautions (5)].
8.5 Geriatric Use
Older patients may be at greater risk of postural hypotension and other serious adverse reactions[see Warnings and Precautions (5)]. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Abuse of tranylcypromine sulfate has been reported. Some of these patients had a history of previous substance abuse.
The potential for abuse and the increased risk of serious adverse reactions with higher doses should be taken into account when considering the use of tranylcypromine sulfate for patients at increased risk for substance abuse.
9.3 Dependence
Dependence, evidenced by precipitation of withdrawal effects following abrupt discontinuation of tranylcypromine sulfate has been reported. Reported withdrawal effects included delirium (even with low daily doses), restlessness, anxiety, confusion, hallucinations, headache, weakness, diarrhea, and/or rapid relapse into depression. Thrombocytopenia and liver enzyme increases have also been observed in association with tranylcypromine sulfate withdrawal from high doses [see Overdosage (10.1)]
Withdrawal effects have appeared within 1 to 3 days of discontinuation and have persisted for several weeks after discontinuation. The use of daily doses greater than recommended and longer duration of use appear to be associated with a higher risk of withdrawal effects.
Monitor for withdrawal effects for at least 1 week after discontinuation. Consider discontinuing tranylcypromine sulfate therapy by slow, gradual dose reduction [see Dosage and Administration (2.3)].
OVERDOSAGE SECTION
10 OVERDOSAGE
10.1 Overdosage Symptoms, Signs, and Laboratory Abnormalities
Overdose of tranylcypromine sulfate can cause the adverse reactions generally associated with tranylcypromine sulfate administration [see Warnings and Precautions (5), Adverse Reactions (6) and Drug Interactions (7.1)]. However, these reactions may be more severe, including fatal reactions. Effects reported with overdosage of tranylcypromine sulfate and/or other MAOIs include:
- Insomnia, restlessness, and anxiety, progressing in severe cases to agitation, mental confusion, and incoherence; delirium; seizures
- Hypotension, dizziness, weakness, and drowsiness, progressing in severe cases to extreme dizziness and shock
- Hypertension with severe headache and other symptoms/complications
- Twitching or myoclonic fibrillation of skeletal muscles, with hyperpyrexia, sometimes progressing to generalized rigidity and coma
10.2 Overdosage Management
There are no specific antidotes for tranylcypromine sulfate. For current information on the management of poisoning or overdosage, contact a poison control center at 1-800-222-1222
Abrupt withdrawal of tranylcypromine sulfate following overdosage can precipitate withdrawal symptoms, including delirium [see Warnings and Precautions 5.9) and Drug Abuse and Dependence (9.3)]
Medical management should normally consist of general supportive measures, close observation of vital signs, and steps to counteract specific manifestations as they occur [see Warnings and Precautions (5)].The toxic effects of tranylcypromine sulfate may be delayed or prolonged following the last dose of the drug [see Clinical Pharmacology (12.2)]. Therefore, the patient should be closely observed for at least 1 week.
Data on the dialyzability of tranylcypromine are lacking.
DESCRIPTION SECTION
11 DESCRIPTION
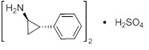
Tranylcypromine sulfate, the active ingredient of Tranylcypromine Sulfate Tablets, USP, is a non-hydrazine MAOI. The chemical name is (±)‑trans‑2‑phenylcyclopropylamine sulfate (2:1). The molecular formula is (C9H11N)2•H2SO4 and its molecular weight is 364.46. The structural formula is:
Tranylcypromine Sulfate film-coated tablets are intended for oral administration. Each round, dark pink, film-coated tablet is debossed with "250" on one side and "K" on the other side and contains tranylcypromine sulfate equivalent to 10 mg of tranylcypromine.
Inactive ingredients consist of colloidal silicon dioxide, croscarmellose sodium, dibasic calcium phosphate anhydrous, magnesium stearate, microcrystalline cellulose, talc, and Opadry® II pink 85F14289. Opadry pink is used for purposes of coating and contains the following: FD&C Red # 40, polyethylene glycol 3350, polyvinyl alcohol, talc and titanium dioxide.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of tranylcypromine sulfate as an antidepressant is not fully understood, but is presumed to be linked to potentiation of monoamine neurotransmitter activity in the central nervous system (CNS) resulting from its irreversible inhibition of the enzyme monoamine oxidase (MAO).
12.2 Pharmacodynamics
Although tranylcypromine is eliminated in 24 hours, recovery MAO activity takes up to 3 to 5 days [see Warnings and Precautions (5.9)].
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.3 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenesis, mutagenesis, or fertility impairment studies were conducted.
