ATORVASTATIN CALCIUM
These highlights do not include all the information needed to use ATORVASTATIN CALCIUM TABLETS safely and effectively. See full prescribing information for ATORVASTATIN CALCIUM TABLETS. ATORVASTATIN CALCIUM tablets, for oral use Initial U.S. Approval: 1996
52d8508b-aa98-cd89-5991-e2b5f982b6c6
HUMAN PRESCRIPTION DRUG LABEL
Jun 14, 2023
NORTHSTAR RX LLC
DUNS: 830546433
Products 4
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
ATORVASTATIN CALCIUM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
ATORVASTATIN CALCIUM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
ATORVASTATIN CALCIUM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
ATORVASTATIN CALCIUM
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Atorvastatin Calcium Tablets are indicated:
- To reduce the risk of:
- Myocardial infarction (MI), stroke, revascularization procedures, and angina in adults with multiple risk factors for coronary heart disease (CHD) but without clinically evident CHD
- MI and stroke in adults with type 2 diabetes mellitus with multiple risk factors for CHD but without clinically evident CHD
- Non-fatal MI, fatal and non-fatal stroke, revascularization procedures, hospitalization for congestive heart failure, and angina in adults with clinically evident CHD
- As an adjunct to diet to reduce low-density lipoprotein cholesterol (LDL-C) in:
- Adults with primary hyperlipidemia.
- Adults and pediatric patients aged 10 years and older with heterozygous familial hypercholesterolemia (HeFH).
- As an adjunct to other LDL-C-lowering therapies, or alone if such treatments are unavailable, to reduce LDL-C in adults and pediatric patients aged 10 years and older with homozygous familial hypercholesterolemia (HoFH).
- As an adjunct to diet for the treatment of adults with:
- Primary dysbetalipoproteinemia
- Hypertriglyceridemia
Atorvastatin calcium tablets are an HMG-CoA reductase inhibitor (statin) indicated (1):
- To reduce the risk of:
- Myocardial infarction (MI), stroke, revascularization procedures, and angina in adults with multiple risk factors for coronary heart disease (CHD) but without clinically evident CHD.
- MI and stroke in adults with type 2 diabetes mellitus with multiple risk factors for CHD but without clinically evident CHD.
- Non-fatal MI, fatal and non-fatal stroke, revascularization procedures, hospitalization for congestive heart failure, and angina in adults with clinically evident CHD.
- As an adjunct to diet to reduce low-density lipoprotein (LDL-C) in:
- Adults with primary hyperlipidemia.
- Adults and pediatric patients aged 10 years and older with heterozygous familial hypercholesterolemia (HeFH).
- As an adjunct to other LDL-C-lowering therapies to reduce LDL-C in adults and pediatric patients aged 10 years and older with homozygous familial hypercholesterolemia.
- As an adjunct to diet for the treatment of adults with:
- Primary dysbetaliproteinemia.
- Hypertriglyceridemia.
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
Atorvastatin calcium may cause myopathy (muscle pain, tenderness, or weakness associated with elevated creatine kinase [CK]) and rhabdomyolysis. Acute kidney injury secondary to myoglobinuria and rare fatalities have occurred as a result of rhabdomyolysis in patients treated with statins, including atorvastatin.
Risk Factors for Myopathy
Risk factors for myopathy include age 65 years or greater, uncontrolled hypothyroidism, renal impairment, concomitant use with certain other drugs (including other lipid-lowering therapies), and higher atorvastatin calcium dosage [see Drug Interactions (7.1) and Use in Specific Populations (8.5, 8.6)].
Steps to Prevent or Reduce the Risk of Myopathy and Rhabdomyolysis
Atorvastatin calcium exposure may be increased by drug interactions due to inhibition of cytochrome P450 enzyme 3A4 (CYP3A4) and/or transporters (e.g., breast cancer resistant protein [BCRP], organic anion-transporting polypeptide [OATP1B1/OATP1B3] and P-glycoprotein [P-gp]), resulting in an increased risk of myopathy and rhabdomyolysis. Concomitant use of cyclosporine, gemfibrozil, tipranavir plus ritonavir, or glecaprevir plus pibrentasvir with atorvastatin is not recommended. Atorvastatin calcium dosage modifications are recommended for patients taking certain anti-viral, azole antifungals, or macrolide antibiotic medications [see Dosage and Administration (2.5)]. Cases of myopathy/rhabdomyolysis have been reported with atorvastatin co-administered with lipid modifying doses (>1 gram/day) of niacin, fibrates, colchicine, and ledipasvir plus sofosbuvir. Consider if the benefit of use of these products outweighs the increased risk of myopathy and rhabdomyolysis [see Drug Interactions (7.1)].
Concomitant intake of large quantities, more than 1.2 liters daily, of grapefruit juice is not recommended in patients taking atorvastatin calcium [see Drug Interactions (7.1)].
Discontinue atorvastatin calcium tablets if markedly elevated CK levels occur or if myopathy is either diagnosed or suspected. Muscle symptoms and CK elevations may resolve if atorvastatin calcium tablets are discontinued. Temporarily discontinue atorvastatin calcium tablets in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis (e.g., sepsis; shock; severe hypovolemia; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy).
Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing the atorvastatin dosage. Instruct patients to promptly report any unexplained muscle pain, tenderness or weakness, particularly if accompanied by malaise or fever.
5.2 Immune-Mediated Necrotizing Myopathy
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use, including reports of recurrence when the same or a different statin was administered. IMNM is characterized by proximal muscle weakness and elevated serum creatine kinase that persists despite discontinuation of statin treatment; positive anti-HMG CoA reductase antibody; muscle biopsy showing necrotizing myopathy; and improvement with immunosuppressive agents. Additional neuromuscular and serologic testing may be necessary. Treatment with immunosuppressive agents may be required. Discontinue atorvastatin calcium tablets if IMNM is suspected.
5.3 Hepatic Dysfunction
Increases in serum transaminases have been reported with use of atorvastatin calcium tablets [see Adverse Reactions (6.1)]. In most cases, these changes appeared soon after initiation, were transient, were not accompanied by symptoms, and resolved or improved on continued therapy or after a brief interruption in therapy. Persistent increases to more than three times the ULN in serum transaminases have occurred in approximately 0.7% of patients receiving atorvastatin calcium tablets in clinical trials. There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including atorvastatin.
Patients who consume substantial quantities of alcohol and/or have a history of liver disease may be at increased risk for hepatic injury [see Use in Specific Populations (8.7)].
Consider liver enzyme testing before atorvastatin calcium tablets initiation and when clinically indicated thereafter. Atorvastatin calcium tablets are contraindicated in patients with acute liver failure or decompensated cirrhosis [see Contraindications (4)]. If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue atorvastatin calcium tablets.
5.4 Increases in HbA1c and Fasting Serum Glucose Levels
Increases in HbA1c and fasting serum glucose levels have been reported with statins, including atorvastatin. Optimize lifestyle measures, including regular exercise, maintaining a healthy body weight, and making healthy food choices.
5.5 Increased Risk of Hemorrhagic Stroke in Patients on Atorvastatin
Calcium Tablets 80 mg with Recent Hemorrhagic Stroke
In a post-hoc analysis of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial where 2365 adult patients, without CHD who had a stroke or TIA within the preceding 6 months, were treated with atorvastatin calcium 80 mg, a higher incidence of hemorrhagic stroke was seen in the atorvastatin calcium 80 mg group compared to placebo (55, 2.3% atorvastatin calcium vs. 33, 1.4% placebo; HR: 1.68, 95% CI: 1.09, 2.59; p=0.0168). The incidence of fatal hemorrhagic stroke was similar across treatment groups (17 vs. 18 for the atorvastatin and placebo groups, respectively). The incidence of non-fatal hemorrhagic stroke was significantly higher in the atorvastatin calcium group (38, 1.6%) as compared to the placebo group (16, 0.7%). Some baseline characteristics, including hemorrhagic and lacunar stroke on study entry, were associated with a higher incidence of hemorrhagic stroke in the atorvastatin calcium group [see Adverse Reactions (6.1)]. Consider the risk/benefit of use of atorvastatin calcium 80 mg in patients with recent hemorrhagic stroke.
- Myopathy and Rhabdomyolysis: Risk factors include age 65 years or greater, uncontrolled hypothyroidism, renal impairment, concomitant use with certain other drugs, and higher atorvastatin calcium dosage. Discontinue atorvastatin calcium tablets if markedly elevated CK levels occur or myopathy is diagnosed or suspected. Temporarily discontinue atorvastatin calcium in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis. Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing atorvastatin calcium dosage. Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever (2.5, 5.1, 7.1, 8.5, 8.6).
- Immune-Mediated Necrotizing Myopathy (IMNM): Rare reports of IMNM, an autoimmune myopathy, have been reported with statin use. Discontinue atorvastatin calcium tablets if IMNM is suspected (5.2).
- Hepatic Dysfunction: Increases in serum transaminases have occurred, some persistent. Rare reports of fatal and non-fatal hepatic failure have occurred. Consider testing liver enzymes before initiating therapy and as clinically indicated thereafter. If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue atorvastatin calcium tablets (5.3).
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
- Take Atorvastatin calcium tablet orally once daily at any time of the day, with or without food.
- Assess LDL-C when clinically appropriate, as early as 4 weeks after initiating atorvastatin calcium tablets, and adjust the dosage if necessary.
2.2 Recommended Dosage in Adult Patients
The recommended starting dosage of atorvastatin calcium is 10 mg to 20 mg once daily. The dosage range is 10 mg to 80 mg once daily. Patients who require reduction in LDL-C greater than 45% may be started at 40 mg once daily.
2.3 Recommended Dosage in Pediatric Patients 10 Years of Age and Older with
HeFH
The recommended starting dosage of atorvastatin calcium is 10 mg once daily. The dosage range is 10 mg to 20 mg once daily.
2.4 Recommended Dosage in Pediatric Patients 10 Years of Age and Older with
HoFH
The recommended starting dosage of atorvastatin calcium is 10 mg to 20 mg once daily. The dosage range is 10 mg to 80 mg once daily.
2.5 Dosage Modifications Due to Drug Interactions
Concomitant use of atorvastatin with the following drugs requires dosage modification of atorvastatin [see Warnings and Precautions (5.1) and Drug Interactions (7.1)].
Anti-Viral Medications
- In patients taking saquinavir plus ritonavir, darunavir plus ritonavir, fosamprenavir, fosamprenavir plus ritonavir, elbasvir plus grazoprevir or letermovir, do not exceed atorvastatin calcium 20 mg once daily.
- In patients taking nelfinavir, do not exceed atorvastatin calcium 40 mg once daily.
Select Azole Antifungals or Macrolide Antibiotics
- In patients taking clarithromycin or itraconazole, do not exceed atorvastatin calcium 20 mg once daily.
For additional recommendations regarding concomitant use of atorvastatin calcium with other anti-viral medications, azole antifungals or macrolide antibiotics, see Drug Interactions (7.1).
- Take orally once daily with or without food (2.1).
- Assess LDL-C when clinically appropriate, as early as 4 weeks after initiating atorvastatin calcium, and adjust dosage if necessary (2.1).
- Adults (2.2):
- Recommended starting dosage is 10 or 20 mg once daily; dosage range is 10 mg to 80 mg once daily.
- Patients requiring LDL-C reduction >45% may start at 40 mg once daily.
- Pediatric Patients Aged 10 Years of Age and Older with HeFH: Recommended starting dosage is 10 mg once daily; dosage range is 10 to 20 mg once daily (2.3).
- Pediatric Patients Aged 10 Years of Age and Older with HoFH: Recommended starting dosage is 10 to 20 mg once daily; dosage range is 10 to 80 mg once daily (2.4).
- See full prescribing information for atorvastatin calcium tablets dosage modifications due to drug interactions (2.5).
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year carcinogenicity study in rats at dose levels of 10, 30, and 100 mg/kg/day, 2 rare tumors were found in muscle in high-dose females: in one, there was a rhabdomyosarcoma and, in another, there was a fibrosarcoma. This dose represents a plasma AUC (0 to 24) value of approximately 16 times the mean human plasma drug exposure after an 80 mg oral dose.
A 2-year carcinogenicity study in mice given 100, 200, or 400 mg/kg/day resulted in a significant increase in liver adenomas in high-dose males and liver carcinomas in high-dose females. These findings occurred at plasma AUC (0 to 24) values of approximately 6 times the mean human plasma drug exposure after an 80 mg oral dose.
In vitro, atorvastatin was not mutagenic or clastogenic in the following tests with and without metabolic activation: the Ames test with Salmonella typhimurium and Escherichia coli, the HGPRT forward mutation assay in Chinese hamster lung cells, and the chromosomal aberration assay in Chinese hamster lung cells. Atorvastatin was negative in the in vivo mouse micronucleus test.
In female rats, atorvastatin at doses up to 225 mg/kg (56 times the human exposure) did not cause adverse effects on fertility. Studies in male rats performed at doses up to 175 mg/kg (15 times the human exposure) produced no changes in fertility. There was aplasia and aspermia in the epididymis of 2 of 10 rats treated with 100 mg/kg/day of atorvastatin for 3 months (16 times the human AUC at the 80 mg dose); testis weights were significantly lower at 30 and 100 mg/kg and epididymal weight was lower at 100 mg/kg. Male rats given 100 mg/kg/day for 11 weeks prior to mating had decreased sperm motility, spermatid head concentration, and increased abnormal sperm. Atorvastatin caused no adverse effects on semen parameters, or reproductive organ histopathology in dogs given doses of 10, 40, or 120 mg/kg for 2 years.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
Prevention of Cardiovascular Disease
In the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), the effect of atorvastatin calcium on fatal and non-fatal coronary heart disease was assessed in 10,305 patients with hypertension, 40 to 80 years of age (mean of 63 years; 19% women; 95% White, 3% Black, 1% South Asian, 1% other), without a previous myocardial infarction and with total cholesterol (TC) levels ≤251 mg/dL. Additionally, all patients had at least 3 of the following cardiovascular risk factors: male gender (81%), age >55 years (85%), smoking (33%), diabetes (24%), history of CHD in a first-degree relative (26%), TC:HDL
6 (14%), peripheral vascular disease (5%), left ventricular hypertrophy (14%), prior cerebrovascular event (10%), specific ECG abnormality (14%), proteinuria/albuminuria (62%). In this double-blind, placebo-controlled trial, patients were treated with antihypertensive therapy (goal BP <140/90 mm Hg for patients without diabetes; <130/80 mm Hg for patients with diabetes) and allocated to either atorvastatin calcium 10 mg daily (n=5,168) or placebo (n=5,137), using a covariate adaptive method which took into account the distribution of nine baseline characteristics of patients already enrolled and minimized the imbalance of those characteristics across the groups. Patients were followed for a median duration of 3.3 years.
The effect of 10 mg/day of atorvastatin calcium on lipid levels was similar to that seen in previous clinical trials.
Atorvastatin calcium significantly reduced the rate of coronary events [either fatal coronary heart disease (46 events in the placebo group vs. 40 events in the atorvastatin calcium group) or non-fatal MI (108 events in the placebo group vs. 60 events in the atorvastatin calcium group)] with a relative risk reduction of 36% [(based on incidences of 1.9% for atorvastatin calcium vs. 3% for placebo), p=0.0005 (see Figure 1)]. The risk reduction was consistent regardless of age, smoking status, obesity, or presence of renal dysfunction. The effect of atorvastatin calcium was seen regardless of baseline LDL levels.
Figure 1: Effect of Atorvastatin Calcium 10 mg/day on Cumulative Incidence of Non-Fatal Myocardial Infarction or Coronary Heart Disease Death (in ASCOT- LLA)
****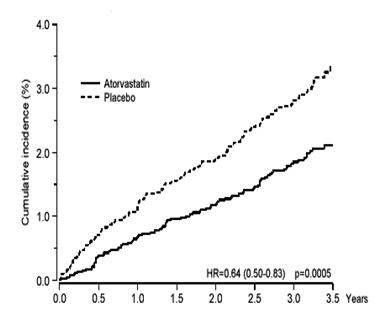
Atorvastatin calcium also significantly decreased the relative risk for revascularization procedures by 42% (incidences of 1.4% for atorvastatin calcium and 2.5% for placebo). Although the reduction of fatal and non-fatal strokes did not reach a pre-defined significance level (p=0.01), a favorable trend was observed with a 26% relative risk reduction (incidences of 1.7% for atorvastatin calcium and 2.3% for placebo). There was no significant difference between the treatment groups for death due to cardiovascular causes (p=0.51) or noncardiovascular causes (p=0.17).
In the Collaborative Atorvastatin Diabetes Study (CARDS), the effect of atorvastatin calcium on cardiovascular disease (CVD) endpoints was assessed in 2,838 subjects (94% White, 2% Black, 2% South Asian, 1% other; 68% male), ages 40 to 75 with type 2 diabetes based on WHO criteria, without prior history of cardiovascular disease and with LDL ≤160 mg/dL and triglycerides (TG) ≤600 mg/dL. In addition to diabetes, subjects had 1 or more of the following risk factors: current smoking (23%), hypertension (80%), retinopathy (30%), or microalbuminuria (9%) or macroalbuminuria (3%). No subjects on hemodialysis were enrolled in the trial. In this multicenter, placebo-controlled, double- blind clinical trial, subjects were randomly allocated to either atorvastatin calcium 10 mg daily (1429) or placebo (1411) in a 1:1 ratio and were followed for a median duration of 3.9 years. The primary endpoint was the occurrence of any of the major cardiovascular events: myocardial infarction, acute CHD death, unstable angina, coronary revascularization, or stroke. The primary analysis was the time to first occurrence of the primary endpoint.
Baseline characteristics of subjects were: mean age of 62 years, mean HbA1c 7.7%; median LDL-C 120 mg/dL; median TC 207 mg/dL; median TG 151 mg/dL; median HDL-C 52 mg/dL.
The effect of atorvastatin calcium 10 mg/day on lipid levels was similar to that seen in previous clinical trials.
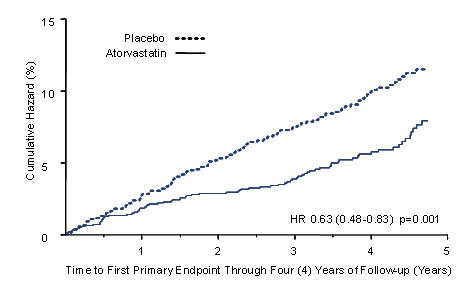
Atorvastatin calcium significantly reduced the rate of major cardiovascular events (primary endpoint events) (83 events in the atorvastatin calcium group vs. 127 events in the placebo group) with a relative risk reduction of 37%, HR 0.63, 95% CI (0.48, 0.83) (p=0.001) (see Figure 2). An effect of atorvastatin calcium was seen regardless of age, sex, or baseline lipid levels.
Atorvastatin calcium significantly reduced the risk of stroke by 48% (21 events in the atorvastatin calcium group vs. 39 events in the placebo group), HR 0.52, 95% CI (0.31, 0.89) (p=0.016) and reduced the risk of MI by 42% (38 events in the atorvastatin calcium group vs. 64 events in the placebo group), HR 0.58, 95.1% CI (0.39, 0.86) (p=0.007). There was no significant difference between the treatment groups for angina, revascularization procedures, and acute CHD death.
There were 61 deaths in the atorvastatin calcium group vs. 82 deaths in the placebo group (HR 0.73, p=0.059).
Figure 2: Effect of Atorvastatin Calcium 10 mg/day on Time to Occurrence of Major Cardiovascular Event (myocardial infarction, acute CHD death, unstable angina, coronary revascularization, or stroke) in CARDS
****
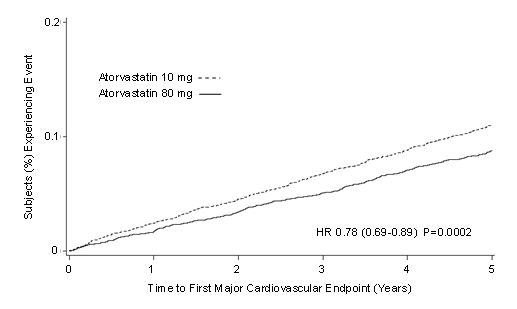
In the Treating to New Targets Study (TNT), the effect of atorvastatin calcium 80 mg/day vs. atorvastatin calcium 10 mg/day on the reduction in cardiovascular events was assessed in 10,001 subjects (94% White, 81% male, 38% ≥65 years) with clinically evident coronary heart disease who had achieved a target LDL-C level <130 mg/dL after completing an 8-week, open-label, run-in period with atorvastatin calcium 10 mg/day. Subjects were randomly assigned to either 10 mg/day or 80 mg/day of atorvastatin calcium and followed for a median duration of 4.9 years. The primary endpoint was the time-to-first occurrence of any of the following major cardiovascular events (MCVE): death due to CHD, non-fatal myocardial infarction, resuscitated cardiac arrest, and fatal and non-fatal stroke. The mean LDL-C, TC, TG, non-HDL, and HDL cholesterol levels at 12 weeks were 73, 145, 128, 98, and 47 mg/dL during treatment with 80 mg of atorvastatin calcium and 99, 177, 152, 129, and 48 mg/dL during treatment with 10 mg of atorvastatin calcium.
Treatment with atorvastatin calcium 80 mg/day significantly reduced the rate of MCVE (434 events in the 80 mg/day group vs. 548 events in the 10 mg/day group) with a relative risk reduction of 22%, HR 0.78, 95% CI (0.69, 0.89), p=0.0002 (see Figure 3 and Table 7). The overall risk reduction was consistent regardless of age (<65, ≥65) or sex.
Figure 3: Effect of Atorvastatin Calcium 80 mg/day vs. 10 mg/day on Time to Occurrence of Major Cardiovascular Events (TNT)
****
|
Endpoint |
Atorvastatin |
Atorvastatin | ||||
|---|---|---|---|---|---|---|
|
10 mg |
80 mg |
HRa (95%CI) | ||||
|
(N=5006) |
(N=4995) | |||||
|
PRIMARY ENDPOINT |
n |
(%) |
n |
(%) | ||
|
First major cardiovascular endpoint |
548 |
(10.9) |
434 |
(8.7) |
0.78 (0.69, 0.89) | |
|
Components of the Primary Endpoint | ||||||
|
CHD death |
127 |
(2.5) |
101 |
(2) |
0.80 (0.61, 1.03) | |
|
Non-fatal, non-procedure related MI |
308 |
(6.2) |
243 |
(4.9) |
0.78 (0.66, 0.93) | |
|
Resuscitated cardiac arrest |
26 |
(0.5) |
25 |
(0.5) |
0.96 (0.56, 1.67) | |
|
Stroke (fatal and non-fatal) |
155 |
(3.1) |
117 |
(2.3) |
0.75 (0.59, 0.96) | |
|
SECONDARY ENDPOINTS* | ||||||
|
First CHF with hospitalization |
164 |
(3.3) |
122 |
(2.4) |
0.74 (0.59, 0.94) | |
|
First PVD endpoint |
282 |
(5.6) |
275 |
(5.5) |
0.97 (0.83, 1.15) | |
|
First CABG or other coronary revascularization procedureb |
904 |
(18.1) |
667 |
(13.4) |
0.72 (0.65, 0.80) | |
|
First documented angina endpointb |
615 |
(12.3) |
545 |
(10.9) |
0.88 (0.79, 0.99) | |
|
All-cause mortality |
282 |
(5.6) |
284 |
(5.7) |
1.01 (0.85, 1.19) | |
|
Components of All-Cause Mortality | ||||||
|
Cardiovascular death |
155 |
(3.1) |
126 |
(2.5) |
0.81 (0.64, 1.03) | |
|
Noncardiovascular death |
127 |
(2.5) |
158 |
(3.2) |
1.25 (0.99, 1.57) | |
|
Cancer death |
75 |
(1.5) |
85 |
(1.7) |
1.13 (0.83, 1.55) | |
|
Other non-CV death |
43 |
(0.9) |
58 |
(1.2) |
1.35 (0.91, 2) | |
|
Suicide, homicide, and other traumatic non-CV death |
9 |
(0.2) |
15 |
(0.3) |
1.67 (0.73, 3.82) | |
|
a Atorvastatin 80 mg: atorvastatin 10 mg b Component of other secondary endpoints
HR=hazard ratio; CHD=coronary heart disease; CI=confidence interval; MI=myocardial infarction; CHF=congestive heart failure; CV=cardiovascular; PVD=peripheral vascular disease; CABG=coronary artery bypass graft Confidence intervals for the Secondary Endpoints were not adjusted for multiple comparisons |
Of the events that comprised the primary efficacy endpoint, treatment with atorvastatin calcium 80 mg/day significantly reduced the rate of non-fatal, non-procedure related MI and fatal and non-fatal stroke, but not CHD death or resuscitated cardiac arrest (Table 7). Of the predefined secondary endpoints, treatment with atorvastatin calcium 80 mg/day significantly reduced the rate of coronary revascularization, angina, and hospitalization for heart failure, but not peripheral vascular disease. The reduction in the rate of CHF with hospitalization was only observed in the 8% of patients with a prior history of CHF.
There was no significant difference between the treatment groups for all-cause mortality (Table 7). The proportions of subjects who experienced cardiovascular death, including the components of CHD death and fatal stroke, were numerically smaller in the atorvastatin calcium 80 mg group than in the atorvastatin calcium 10 mg treatment group. The proportions of subjects who experienced noncardiovascular death were numerically larger in the atorvastatin calcium 80 mg group than in the atorvastatin calcium 10 mg treatment group.
Primary Hyperlipidemia in Adults
Atorvastatin calcium reduces total-C, LDL-C, apo B, and TG, and increases HDL-C in patients with hyperlipidemia (heterozygous familial and nonfamilial) and mixed dyslipidemia. Therapeutic response is seen within 2 weeks, and maximum response is usually achieved within 4 weeks and maintained during chronic therapy.
In two multicenter, placebo-controlled, dose-response trials in patients with hyperlipidemia, atorvastatin calcium given as a single dose over 6 weeks, significantly reduced total-C, LDL-C, apo B, and TG. (Pooled results are provided in Table 8.)
**Table 8: Dose Response in Patients with Primary Hyperlipidemia (Adjusted Mean % Change From Baseline)**a
|
Dose |
N |
TC |
LDL-C |
Apo B |
TG |
HDL-C |
|
Placebo |
21 |
4 |
4 |
3 |
10 |
-3 |
|
10 |
22 |
-29 |
-39 |
-32 |
-19 |
6 |
|
20 |
20 |
-33 |
-43 |
-35 |
-26 |
9 |
|
40 |
21 |
-37 |
-50 |
-42 |
-29 |
6 |
|
80 |
23 |
-45 |
-60 |
-50 |
-37 |
5 |
a Results are pooled from 2 dose-response trials.
In three multicenter, double-blind trials in patients with hyperlipidemia, atorvastatin calcium was compared to other statins. After randomization, patients were treated for 16 weeks with either atorvastatin calcium 10 mg per day or a fixed dose of the comparative agent (Table 9).
Table 9: Mean Percentage Change From Baseline at Endpoint (Double-Blind, Randomized, Active-Controlled Trials)
|
Treatment (Daily Dose) |
N |
Total-C |
LDL-C |
Apo B |
TG |
HDL-C |
|
Trial 1 | ||||||
|
Atorvastatin 10 mg |
707 |
-27a |
-36 a |
-28 a |
-17 a |
+7 |
|
Lovastatin 20 mg |
191 |
-19 |
-27 |
-20 |
-6 |
+7 |
|
95% CI for Diff1 |
-9.2, -6.5 |
-10.7, -7.1 |
-10, -6.5 |
-15.2, -7.1 |
-1.7, 2 | |
|
Trial 2 | ||||||
|
Atorvastatin 10 mg |
222 |
-25b |
-35 b |
-27 b |
-17 b |
+6 |
|
Pravastatin 20 mg |
77 |
-17 |
-23 |
-17 |
-9 |
+8 |
|
95% CI for Diff1 |
-10.8, -6.1 |
-14.5, -8.2 |
-13.4, -7.4 |
-14.1, -0.7 |
-4.9, 1.6 | |
|
Trial 3 | ||||||
|
Atorvastatin 10 mg |
132 |
-29c |
-37 c |
-34 c |
-23 c |
+7 |
|
Simvastatin 10 mg |
45 |
-24 |
-30 |
-30 |
-15 |
+7 |
|
95% CI for Diff1 |
-8.7, -2.7 |
-10.1, -2.6 |
-8, -1.1 |
-15.1, -0.7 |
-4.3, 3.9 |
1 A negative value for the 95% CI for the difference between treatments favors atorvastatin for all except HDL-C, for which a positive value favors atorvastatin. If the range does not include 0, this indicates a statistically significant difference.
a Significantly different from lovastatin, ANCOVA, p ≤0.05
b Significantly different from pravastatin, ANCOVA, p ≤0.05
c Significantly different from simvastatin, ANCOVA, p ≤0.05
Table 9 does not contain data comparing the effects of atorvastatin 10 mg and higher doses of lovastatin, pravastatin, and simvastatin. The drugs compared in the trials summarized in the table are not necessarily interchangeable.
Hypertriglyceridemia in Adults
The response to atorvastatin calcium in 64 patients with isolated hypertriglyceridemia treated across several clinical trials is shown in the table below (Table 10). For the atorvastatin calcium-treated patients, median (min, max) baseline TG level was 565 (267 to 1502).
Table 10: Combined Patients with Isolated Elevated TG: Median (min, max) Percentage Change From Baseline|
Placebo |
Atorvastatin 10 mg |
Atorvastatin 20 mg |
Atorvastatin 80 mg | |
|
Triglycerides |
-12.4 (-36.6, 82.7) |
-41 (-76.2, 49.4) |
-38.7 (-62.7, 29.5) |
-51.8 (-82.8, 41.3) |
|
Total-C |
-2.3 (-15.5, 24.4) |
-28.2 (-44.9, -6.8) |
-34.9 (-49.6, -15.2) |
-44.4 (-63.5, -3.8) |
|
LDL-C |
3.6 (-31.3, 31.6) |
-26.5 (-57.7, 9.8) |
-30.4 (-53.9, 0.3) |
-40.5 (-60.6, -13.8) |
|
HDL-C |
3.8 (-18.6, 13.4) |
13.8 (-9.7, 61.5) |
11 (-3.2, 25.2) |
7.5 (-10.8, 37.2) |
|
non-HDL-C |
-2.8 (-17.6, 30) |
-33 (-52.1, -13.3) |
-42.7 (-53.7, -17.4) |
-51.5 (-72.9, -4.3) |
Dysbetalipoproteinemia in Adults
The results of an open-label crossover trial of 16 patients (genotypes: 14 apo E2/E2 and 2 apo E3/E2) with dysbetalipoproteinemia are shown in the table below (Table 11).
Table 11: Open-Label Crossover Trial of 16 Patients with Dysbetalipoproteinemia (Fredrickson Type III)|
Median % Change (min, max) | |||
|
Median (min, max) at |
Atorvastatin |
Atorvastatin | |
|
Total-C |
442 (225, 1320) |
-37 (-85, 17) |
-58 (-90, -31) |
|
Triglycerides |
678 (273, 5990) |
-39 (-92, -8) |
-53 (-95, -30) |
|
IDL-C + VLDL-C |
215 (111, 613) |
-32 (-76, 9) |
-63 (-90, -8) |
|
non-HDL-C |
411 (218, 1272) |
-43 (-87, -19) |
-64 (-92, -36) |
HoFH in Adults and Pediatric Patients
In a trial without a concurrent control group, 29 patients (mean age of 22 years, median age of 24 years, 31% <18 years) with HoFH received maximum daily doses of 20 to 80 mg of atorvastatin calcium. The mean LDL-C reduction in this trial was 18%. Twenty-five patients with a reduction in LDL-C had a mean response of 20% (range of 7% to 53%, median of 24%); the remaining 4 patients had 7% to 24% increases in LDL-C. Five of the 29 patients had absent LDL- receptor function. Of these, 2 patients also had a portacaval shunt and had no significant reduction in LDL-C. The remaining 3 receptor-negative patients had a mean LDL-C reduction of 22%.
HeFH in Pediatric Patients
In a double-blind, placebo-controlled trial followed by an open-label phase, 187 boys and post-menarchal girls 10 years to 17 years of age (mean age 14.1 years; 31% female; 92% White, 1.6% Blacks, 1.6% Asians, 4.8% other) with heterozygous familial hypercholesterolemia (HeFH) or severe hypercholesterolemia, were randomized to atorvastatin calcium (n=140) or placebo (n=47) for 26 weeks and then all received atorvastatin calcium for 26 weeks. Inclusion in the trial required 1) a baseline LDL-C level ≥190 mg/dL or 2) a baseline LDL-C level ≥160 mg/dL and positive family history of FH or documented premature cardiovascular disease in a first or second-degree relative. The mean baseline LDL-C value was 219 mg/dL (range: 139 to 385 mg/dL) in the atorvastatin calcium group compared to 230 mg/dL (range: 160 to 325 mg/dL) in the placebo group. The dosage of atorvastatin calcium (once daily) was 10 mg for the first 4 weeks and uptitrated to 20 mg if the LDL-C level was >130 mg/dL. The number of atorvastatin calcium-treated patients who required uptitration to 20 mg after Week 4 during the double-blind phase was 78 (56%).
Atorvastatin calcium significantly decreased plasma levels of total-C, LDL-C, triglycerides, and apolipoprotein B during the 26-week double-blind phase (see Table 12).
Table 12: Lipid-altering Effects of Atorvastatin Calcium in Adolescent Boys and Girls with Heterozygous Familial Hypercholesterolemia or Severe Hypercholesterolemia (Mean Percentage Change From Baseline at Endpoint in Intention-to-Treat Population)|
DOSAGE |
N |
Total-C |
LDL-C |
HDL-C |
TG |
Apolipoprotein B |
|
Placebo |
47 |
-1.5 |
-0.4 |
-1.9 |
1 |
0.7 |
|
Atorvastatin Calcium Tablets |
140 |
-31.4 |
-39.6 |
2.8 |
-12 |
-34 |
The mean achieved LDL-C value was 130.7 mg/dL (range: 70 to 242 mg/dL) in the atorvastatin calcium group compared to 228.5 mg/dL (range: 152 to 385 mg/dL) in the placebo group during the 26-week double-blind phase.
Atorvastatin was also studied in a three year open-label, uncontrolled trial that included 163 patients with HeFH who were 10 years to 15 years old (82 boys and 81 girls). All patients had a clinical diagnosis of HeFH confirmed by genetic analysis (if not already confirmed by family history). Approximately 98% were White, and less than 1% were Black or Asian. Mean LDL-C at baseline was 232 mg/dL. The starting atorvastatin dosage was 10 mg once daily and doses were adjusted to achieve a target of <130 mg/dL LDL-C. The reductions in LDL-C from baseline were generally consistent across age groups within the trial as well as with previous clinical trials in both adult and pediatric placebo- controlled trials.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Atorvastatin calcium tablets, USP are supplied as white to off-white, oval, biconvex film-coated tablets of atorvastatin calcium containing 10, 20, 40 and 80 mg atorvastatin.
10 mg tablets
Atorvastatin calcium tablets, USP 10 mg, are available for oral administration as white to off-white, oval, biconvex film-coated tablets, engraved “APO” on one side, “A10” on the other side.
|
NDC 16714-173-01 |
90 count |
|
NDC 16714-173-02 |
500 count |
|
NDC 16714-173-03 |
1000 count |
20 mg tablets
Atorvastatin calcium tablets, USP 20 mg, are available for oral administration as white to off-white, oval, biconvex film-coated tablets, engraved “APO” on one side, “ATV20” on the other side.
|
NDC 16714-174-01 |
90 count |
|
NDC 16714-174-02 |
500 count |
|
NDC 16714-174-03 |
1000 count |
40 mg tablets
Atorvastatin calcium tablets, USP 40 mg, are available for oral administration as white to off-white, oval, biconvex film-coated tablets, engraved “APO” on one side, “ATV40” on the other side.
|
NDC 16714-175-01 |
90 count |
|
NDC 16714-175-02 |
500 count |
|
NDC 16714-175-03 |
1000 count |
80 mg tablets
Atorvastatin calcium tablets, USP 80 mg, are available for oral administration as white to off-white, oval, biconvex film-coated tablets, engraved “APO” on one side, “ATV80” on the other side.
|
NDC 16714-176-01 |
90 count |
|
NDC 16714-176-02 |
500 count |
|
NDC 16714-176-03 |
1000 count |
StorageStore at 20°C to 25°C (68°F to 77°F); excursions permitted from 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Dispense in a tight container [see USP].
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Myopathy and Rhabdomyolysis
Advise patients that atorvastatin may cause myopathy and rhabdomyolysis. Inform patients that the risk is also increased when taking certain types of medication or consuming large quantities of grapefruit juice and they should discuss all medication, both prescription and over the counter, with their healthcare provider. Instruct patients to promptly report any unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever [see Warnings and Precautions (5.1), Drug Interactions (7.1)].
Hepatic Dysfunction
Inform patients that atorvastatin calcium tablets may cause liver enzyme elevations and possibly liver failure. Advise patients to promptly report fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice [see Warnings and Precautions (5.3)].
Increases in HbA1c and Fasting Serum Glucose Levels
Inform patients that increases in HbA1c and fasting serum glucose levels may occur with atorvastatin calcium tablets. Encourage patients to optimize lifestyle measures, including regular exercise, maintaining a healthy body weight, and making healthy food choices [see Warnings and Precautions (5.4)].
Pregnancy
Advise pregnant patients and patients who can become pregnant of the potential risk to a fetus. Advise patients to inform their healthcare provider of a known or suspected pregnancy to discuss if atorvastatin calcium tablets should be discontinued [see Use in Specific Populations (8.1)].
Lactation
Advise patients that breastfeeding is not recommended during treatment with atorvastatin calcium tablets [see Use in Specific Populations (8.2)].
All registered trademarks in this document are the property of their respective owners.
|
Manufactured For |
Manufactured By |
|
Northstar Rx LLC |
Apotex Inc. |
|
Memphis, TN 38141 |
Toronto, Ontario |
|
Canada M9L 1T9 |
Rev. 22
