Bupivacaine HCl
These highlights do not include all the information needed to use BUPIVACAINE HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for BUPIVACAINE HYDROCHLORIDE INJECTION. BUPIVACAINE HYDROCHLORIDE injection, for infiltration, perineural, caudal, epidural, or retrobulbar use Initial U.S. Approval: 1972
3335dabe-66d5-440b-a59a-b62993030e0f
HUMAN PRESCRIPTION DRUG LABEL
Jun 9, 2023
Xellia Pharmaceuticals USA LLC
DUNS: 116768762
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Bupivacaine Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (1)
Bupivacaine Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (1)
Drug Labeling Information
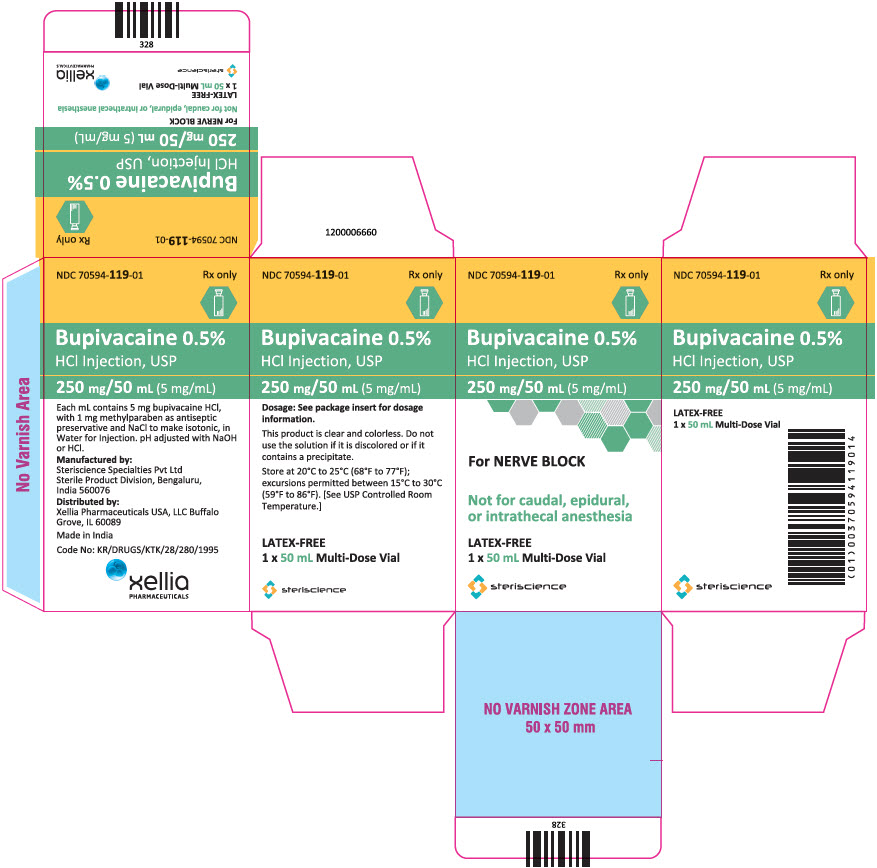
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 250 mg/50 mL Vial Carton
NDC 70594-119-01
Rx only
Bupivacaine 0.5%
HCl Injection, USP
250 mg/50 mL (5 mg/mL)
For NERVE BLOCK
Not for caudal, epidural,
or intrathecal anesthesia
LATEX-FREE
1 x 50 mL Multi-Dose Vial
steriscience
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Bupivacaine hydrochloride injection is indicated in adults for the production of local or regional anesthesia or analgesia for surgery and oral surgery procedures, diagnostic and therapeutic procedures, and for obstetrical procedures. Specific concentrations and presentations of bupivacaine hydrochloride injection are recommended for each type of block indicated to produce local or regional anesthesia or analgesia [see Dosage and Administration (2.2)].
Limitations of Use
Not all blocks are indicated for use with bupivacaine hydrochloride injection given clinically significant risks associated with use [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.1, 5.4, 5.5, 5.7, 5.9)].
Bupivacaine hydrochloride injection contains bupivacaine, an amide local anesthetic. Bupivacaine hydrochloride injection is indicated in adults for the production of local or regional anesthesia or analgesia for surgery and oral surgery procedures, diagnostic and therapeutic procedures, and for obstetrical procedures. For each type of block indicated to produce local or regional anesthesia or analgesia, specific concentrations and presentations are recommended. (1, 2.2)
Limitations of Use
Not all blocks are indicated for use with bupivacaine hydrochloride injection given clinically significant risks associated with use. (1, 2.2, 4, 5.1, 5.4, 5.5, 5.7, 5.9)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Cardiac Arrest with Use of Bupivacaine Hydrochloride Injection
in Obstetrical Anesthesia
There have been reports of cardiac arrest with difficult resuscitation or death during use of bupivacaine hydrochloride injection for epidural anesthesia in obstetrical patients. In most cases, this has followed use of the 0.75% (7.5 mg/mL) concentration. Resuscitation has been difficult or impossible despite apparently adequate preparation and appropriate management. Cardiac arrest has occurred after convulsions resulting from systemic toxicity, presumably following unintentional intravascular injection.
5.2 Dose-Related Toxicity
The safety and effectiveness of bupivacaine hydrochloride injection depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient's state of consciousness should be performed after injection of bupivacaine hydrochloride injection solutions.
Possible early warning signs of central nervous system (CNS) toxicity are restlessness, anxiety, incoherent speech, lightheadedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, CNS depression, or drowsiness. Delay in proper management of dose-related toxicity, underventilation from any cause, and/or altered sensitivity may lead to the development of acidosis, cardiac arrest, and, possibly, death.
During major regional nerve blocks, such as those of the brachial plexus or lower extremity, the patient should have an indwelling intravenous catheter to assure adequate intravenous access. Use the lowest dosage of bupivacaine hydrochloride injection that results in effective anesthesia to avoid high plasma levels and serious adverse effects. Avoid rapid injection of a large volume of bupivacaine hydrochloride injection solution and administer fractional (incremental) doses when feasible.
Injection of repeated doses of bupivacaine hydrochloride injection may cause significant increases in plasma levels with each repeated dose due to slow accumulation of the drug or its metabolites, or to slow metabolic degradation. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients and acutely ill patients should be given reduced doses commensurate with their age and physical status.
5.3 Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition [see Drug Interactions (7.5)]. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious CNS and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue bupivacaine hydrochloride injection and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
5.4 Antimicrobial Preservatives in Multiple-Dose Vials
Avoid use of bupivacaine hydrochloride injection solutions containing antimicrobial preservatives, i.e., those supplied in multiple-dose vials, for epidural or caudal anesthesia because safety has not been established with such use.
5.5 Chondrolysis with Intra-Articular Infusion
Intra-articular infusions of local anesthetics including bupivacaine hydrochloride injection following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric and adult patients following intra-articular infusions of local anesthetics periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are associated with chondrolysis. The time of onset of symptoms, such as joint pain, stiffness and loss of motion can be variable, but may begin as early as the 2nd month after surgery. Currently, there is no effective treatment for chondrolysis; patients who experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
5.7 Risk of Cardiac Arrest with Intravenous Regional Anesthesia Use (Bier
Block)
There have been reports of cardiac arrest and death during the use of bupivacaine for intravenous regional anesthesia (Bier Block). Information on safe dosages and techniques of administration of bupivacaine hydrochloride injection in this procedure is lacking. Therefore, bupivacaine hydrochloride injection is contraindicated for use with this technique [see Contraindications (4)].
5.9 Risk of Systemic Toxicities with Unintended Intravascular or
Intrathecal Injection
Unintended intravascular or intrathecal injection of bupivacaine hydrochloride injection may be associated with systemic toxicities, including CNS or cardiorespiratory depression and coma, progressing ultimately to respiratory arrest. Unintentional intrathecal injection during the intended performance of caudal or lumbar epidural block or nerve blocks near the vertebral column has resulted in underventilation or apnea ("Total or High Spinal"). A high spinal has been characterized by paralysis of the legs, loss of consciousness, respiratory paralysis, and bradycardia [see Adverse Reactions (6)].
Aspirate for blood or cerebrospinal fluid (where applicable) before injecting bupivacaine hydrochloride injection, the initial dose and all subsequent doses, to avoid intravascular or intrathecal injection. However, a negative aspiration for blood or cerebrospinal fluid does not ensure against an intravascular or intrathecal injection.
5.10 Risk of Toxicity in Patients with Hepatic Impairment
Because amide local anesthetics such as bupivacaine are metabolized by the liver, consider reduced dosing and increased monitoring for bupivacaine systemic toxicity in patients with moderate to severe hepatic impairment who are treated with bupivacaine hydrochloride injection, especially with repeat doses [see Use in Specific Populations (8.6)].
5.11 Risk of Use in Patients with Impaired Cardiovascular Function
Bupivacaine hydrochloride injection, should be given in reduced doses in patients with impaired cardiovascular function (e.g., hypotension, heartblock) because they may be less able to compensate for functional changes associated with the prolongation of AV conduction produced by bupivacaine hydrochloride injection. Monitor patients closely for blood pressure, heart rate, and ECG changes.
5.14 Risk of Adverse Reactions with Use in Head and Neck Area
Small doses of local anesthetics (e.g., bupivacaine hydrochloride injection) injected into the head and neck area, including retrobulbar and stellate ganglion blocks, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. The injection procedures require the utmost care.
Confusion, convulsions, respiratory depression, and/or respiratory arrest, and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. They may also be due to puncture of the dural sheath of the optic nerve during retrobulbar block with diffusion of any local anesthetic along the subdural space to the midbrain. Monitor circulation and respiration and constantly observe patients receiving bupivacaine hydrochloride injection blocks. Resuscitative equipment and drugs, and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded [see Dosage and Administration (2.2)].
5.15 Risk of Respiratory Arrest with Use in Ophthalmic Surgery
Clinicians who perform retrobulbar blocks should be aware that there have been reports of respiratory arrest following local anesthetic injection. Prior to retrobulbar block (e.g., with bupivacaine hydrochloride injection), as with all other regional procedures, resuscitative equipment and drugs, and personnel to manage respiratory arrest or depression, convulsions, and cardiac stimulation or depression should be immediately available [see Warnings and Precautions (5.14)]. As with other anesthetic procedures, patients should be constantly monitored following ophthalmic blocks for signs of these adverse reactions, which may occur following relatively low total doses.
- Dose-Related Toxicity: Monitor cardiovascular and respiratory vital signs and patient's state of consciousness after injection of bupivacaine hydrochloride injection. (5.2)
- Methemoglobinemia: Cases of methemoglobinemia have been reported in association with local anesthetic use. See full prescribing information for more detail on managing these risks. (5.3)
- Chondrolysis with Intra-Articular Infusion: Intra-articular infusions of local anesthetics including bupivacaine hydrochloride injection following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. (5.5)
- Risk of Cardiac Arrest with Intravenous Regional Anesthesia Use (Bier Block): There have been reports of cardiac arrest and death during the use of bupivacaine for intravenous regional anesthesia (Bier Block). (5.7)
- Risk of Systemic Toxicities with Unintended Intravascular or Intrathecal Injection: Unintended intravascular or intrathecal injection may be associated with systemic toxicities, including CNS or cardiorespiratory depression and coma, progressing ultimately to respiratory arrest. Aspirate for blood or cerebrospinal fluid (where applicable) prior to each dose. (5.9)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Local Anesthetics
The toxic effects of local anesthetics are additive. If coadministration of other local anesthetics with bupivacaine hydrochloride injection cannot be avoided, monitor patients for neurologic and cardiovascular effects related to local anesthetic systemic toxicity [see Dosage and Administration (2.1), Warnings and Precautions (5.2)].
7.5 Drugs Associated with Methemoglobinemia
Patients who are administered bupivacaine hydrochloride injection are at increased risk of developing methemoglobinemia when concurrently exposed to following drugs, which could include other local anesthetics [see Warnings and Precautions (5.3)].
Examples of Drugs Associated with Methemoglobinemia:
|
Class |
Examples |
|---|---|
|
Nitrates/Nitrites |
nitric oxide, nitroglycerin, nitroprusside, nitrous oxide |
|
Local anesthetics |
articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine |
|
Antineoplastic agents |
cyclophosphamide, flutamide, hydroxyurea, isofamide, rasburicase |
|
Antibiotics |
dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides |
|
Antimalarials |
chloroquine, primaquine |
|
Anticonvulsants |
phenobarbital, phenytoin, sodium valproate |
|
Other drugs |
acetaminophen, metoclopramide, quinine, sulfasalazine |
- Local Anesthetics: The toxic effects of local anesthetics are additive. Monitor for neurologic and cardiovascular effects when additional local anesthetics are administered. (7.1)
- Drugs Associated with Methemoglobinemia: Patients are at increased risk of developing methemoglobinemia when concurrently exposed to nitrates, nitrites, local anesthetics, antineoplastic agents, antibiotics, antimalarials, anticonvulsants, and other drugs. (7.5)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
- Bupivacaine hydrochloride injection is not for intrathecal use.
- Avoid use of bupivacaine hydrochloride injection solutions containing antimicrobial preservatives (i.e., multiple-dose vials) for epidural or caudal anesthesia [see Warnings and Precautions (5.4)].
- Discard unused portions of solution not containing preservatives, i.e., those supplied in single-dose vials, following initial use.
- Visually inspect this product for particulate matter and discoloration prior to administration whenever solution and container permit. Bupivacaine hydrochloride injection is clear, colorless solutions. Do not administer solutions which are discolored or contain particulate matter.
- Mixing or the prior or intercurrent use of any other local anesthetic with bupivacaine hydrochloride injection is not recommended because of insufficient data on the clinical use of such mixtures.
Administration Precautions
- Bupivacaine hydrochloride injection is to be administered in carefully adjusted dosages by or under the supervision of experienced clinicians who are well versed in the diagnosis and management of dose-related toxicity and other acute emergencies which might arise from the block to be employed.
- Use bupivacaine hydrochloride injection only if the following are immediately available: oxygen, cardiopulmonary resuscitative equipment and drugs, and the personnel resources needed for proper management of toxic reactions and related emergencies [see Warnings and Precautions (5.2), Adverse Reactions (6), Overdosage (10)].
- The toxic effects of local anesthetics are additive. Monitor for neurologic and cardiovascular effects related to local anesthetic systemic toxicity when additional local anesthetics are administered with bupivacaine hydrochloride injection [see Warnings and Precautions (5.2), Drug Interactions (7.1), Overdosage (10)].
- Aspirate for blood or cerebrospinal fluid (where applicable) prior to injecting bupivacaine hydrochloride injection the initial dose and all subsequent doses, to avoid intravascular or intrathecal injection. However, a negative aspiration for blood or cerebrospinal fluid does not ensure against an intravascular or intrathecal injection [see Warnings and Precautions (5.9)].
- Avoid rapid injection of a large volume of bupivacaine hydrochloride injection and use fractional (incremental) doses when feasible.
- During major regional nerve blocks, such as those of the brachial plexus or lower extremity, the patient should have an indwelling intravenous catheter to assure adequate intravenous access. The lowest dosage of bupivacaine hydrochloride injection that results in effective anesthesia should be used to avoid high plasma levels and serious adverse reactions.
- Perform careful and constant monitoring of cardiovascular and respiratory (adequacy of oxygenation and ventilation) vital signs and the patient's level of consciousness after each local anesthetic injection.
2.2 Recommended Concentrations and Dosages of bupivacaine hydrochloride
injection
The dosage of bupivacaine hydrochloride injection administered varies with the anesthetic procedure, the area to be anesthetized, the vascularity of the tissues, the number of neuronal segments to be blocked, the depth of anesthesia and degree of muscle relaxation required, the duration of anesthesia desired, individual tolerance, and the physical condition of the patient. Administer the smallest dosage and concentration required to produce the desired result.
The types of block and recommended bupivacaine hydrochloride injection concentrations are shown in Table 1.
Table 1. Types of Block and Recommended bupivacaine hydrochloride injection Concentrations|
Type of Block |
Bupivacaine hydrochloride injection | |
|---|---|---|
|
0.25% (2.5 mg/mL) |
0.5% (5 mg/mL) | |
|
✔ = indicated use [see Warnings and Precautions (5.1)]. | ||
| ||
|
Local infiltration |
✔ | |
|
Peripheral nerve block |
✔ |
✔ |
|
Retrobulbar block | ||
|
Sympathetic block |
✔ | |
|
Caudal block* |
✔ |
✔ |
|
Lumbar epidural block* |
✔ |
✔ |
At recommended dosages, bupivacaine hydrochloride injection produces complete sensory block, but the effect on motor function differs among the three concentrations. Table 2 provides information on the expected effect on motor function for the three concentrations.
Table 2. Bupivacaine Hydrochloride Injection Concentration vs. Motor Function|
Bupivacaine Hydrochloride Injection Concentration |
Motor Function |
|---|---|
|
0.25% |
When used for caudal, epidural, or peripheral nerve block, produces incomplete motor block. Should be used for operations in which muscle relaxation is not important, or when another means of providing muscle relaxation is used concurrently. Onset of action may be slower than with the 0.5% (5 mg/mL). |
|
0.5% |
Provides motor blockade for caudal, epidural, or nerve block, but muscle relaxation may be inadequate for operations in which complete muscle relaxation is essential. |
The duration of anesthesia with bupivacaine hydrochloride injection is such that for most indications, a single-dose is sufficient.
The maximum dosage limit within the recommended dosage range must be individualized in each case after evaluating the size and physical status of the patient, as well as the anticipated rate of systemic absorption from a particular injection site.
The dosages in Table 3 are recommended as a guide for use in the average adult. These doses may be repeated once every three hours. Do not exceed a total daily dosage of 400 mg in 24 hours. The duration of anesthetic effect may be prolonged by the addition of epinephrine.
Table 3. Recommended Concentrations and Doses of bupivacaine hydrochloride injection in Adults|
Type of Block |
Concentration of Bupivacaine Hydrochloride Injection |
Each Dose |
Motor Block* | |
|---|---|---|---|---|
|
mL |
mg of Bupivacaine Hydrochloride Injection | |||
| ||||
|
Local infiltration |
0.25% (2.5 mg/mL)† |
Up to 70 (without epinephrine) |
Up to 175 (without epinephrine) |
— |
|
Peripheral nerve block |
0.5% (5 mg/mL)† |
5-35 (without epinephrine) |
25-175 (without epinephrine) |
moderate to complete |
|
0.25% (2.5 mg/mL)† |
5-70 (without epinephrine) |
12.5-175 (without epinephrine) |
moderate to complete | |
|
Sympathetic block |
0.25% (2.5 mg/mL) |
20-50 |
50-125 |
— |
|
Caudal block |
0.5% (5 mg/mL)† |
15-30 |
75-150 |
moderate to complete |
|
0.25% (2.5 mg/mL)† |
15-30 |
37.5-75 |
moderate | |
|
Lumbar epidural block |
0.5% (5 mg/mL)† |
10-20 |
50-100 |
moderate to complete |
|
0.25% (2.5 mg/mL)† |
10-20 |
25-50 |
partial to moderate |
2.3 Use in Epidural Anesthesia
During epidural administration, administer bupivacaine hydrochloride injection slowly, with frequent aspirations before and during the injection to avoid intravascular injection. Perform syringe aspirations before and during each supplemental injection in continuous (intermittent) catheter techniques. In obstetrics, use ONLY the 0.5% (5 mg/mL) and 0.25% (2.5 mg/mL) concentrations of bupivacaine hydrochloride injection [see Warnings and Precautions (5.1)]; incremental doses of 3 mL to 5 mL of the 0.5% (5 mg/mL) solution not exceeding 50 mg to 100 mg at any dosing interval are recommended. Use only the single- dose vials for caudal or epidural anesthesia; avoid use of the multiple-dose vials for these procedures, which contain a preservative [see Dosage and Administration (2.1, 2.4), Warnings and Precautions (5.4, 5.9)].
- Not for intrathecal use. (2.1)
- Avoid use of solutions containing antimicrobial preservatives (i.e., multiple-dose vials) for epidural or caudal anesthesia. (2.1, 5.4)
- See full prescribing information for:
—
Recommended concentrations and dosages of bupivacaine hydrochloride injection according to type of block. (2.2)
—
Additional dosage and administration information pertaining to use in epidural anesthesia and use in ophthalmic surgery. (2.3, 2.4, 2.5)
OVERDOSAGE SECTION
10 OVERDOSAGE
Clinical Presentation
Acute emergencies from use of bupivacaine hydrochloride injection are generally related to high plasma levels encountered during therapeutic use or to unintended intrathecal injection [see Warnings and Precautions (5.2, 5.9), Adverse Reactions (6)].
If not treated immediately, convulsions with simultaneous hypoxia, hypercarbia, and acidosis plus myocardial depression from the direct effects of bupivacaine may result in cardiac arrhythmias, bradycardia, asystole, ventricular fibrillation, or cardiac arrest. Respiratory abnormalities, including apnea, may occur. Hypoventilation or apnea due to unintentional intrathecal injection of bupivacaine hydrochloride injection may produce these same signs and also lead to cardiac arrest if ventilatory support is not instituted. If cardiac arrest should occur, successful outcome may require prolonged resuscitative efforts.
Management
The first step in the management of systemic toxic reactions, as well as hypoventilation or apnea due to unintentional intrathecal injection of bupivacaine hydrochloride injection, consists of immediate attention to the establishment and maintenance of a patent airway and effective assisted or controlled ventilation with 100% oxygen with a delivery system capable of permitting immediate positive airway pressure by mask. Endotracheal intubation, using drugs and techniques familiar to the clinician, may be indicated after initial administration of oxygen by mask if difficulty is encountered in the maintenance of a patent airway, or if prolonged ventilatory support (assisted or controlled) is indicated.
If necessary, use drugs to manage the convulsions. A bolus intravenous dose of a benzodiazepine will counteract CNS stimulation related to bupivacaine hydrochloride injection. Immediately after the institution of ventilatory measures, evaluate the adequacy of the circulation. Supportive treatment of circulatory depression may require Advance Cardiac Life Support measures.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate the carcinogenic potential of bupivacaine hydrochloride have not been conducted.
Mutagenesis
The mutagenic potential of bupivacaine hydrochloride has not been determined.
Impairment of Fertility
The effect of bupivacaine on fertility has not been determined.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Store at 20 °C to 25 °C (68 °F to 77 °F); excursions permitted between 15 °C to 30 °C (59 ° F to 86 °F). [See USP Controlled Room Temperature.]
Protect from light. This product is clear and colorless. Do not use the solution if it is discolored or if it contains a precipitate.
|
Unit of Sale |
Concentration |
Each |
|---|---|---|
|
0.25% Contains 2.5 mg bupivacaine hydrochloride per mL. | ||
|
NDC 70594-116-01 |
125 mg/50 mL |
NDC 70594-116-01 |
|
Carton of 1 |
(2.5 mg/mL) |
multiple-dose vial |
|
0.5% Contains 5 mg bupivacaine hydrochloride per mL. | ||
|
NDC 70594-119-01 |
250 mg/50 mL |
NDC 70594-119-01 |
|
Carton of 1 |
(5 mg/mL) |
multiple-dose vial |
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Allergic-Type Reactions
Assess if the patient has had allergic-type reactions to amide-type local anesthetics or to other formulation ingredients, such as the antimicrobial preservative methylparaben contained in multiple-dose vials [see Contraindications (4), Adverse Reactions (6)].
Temporary Loss of Sensation and Motor Activity After Caudal or Epidural Anesthesia
When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body, following proper administration of caudal or epidural anesthesia.
Methemoglobinemia
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue [see Warnings and Precautions (5.3)].
