Diabecin HR
NDC 59088-790 Diabecin HR
36c60fe2-5b7b-83dd-e063-6294a90ad467
HUMAN PRESCRIPTION DRUG LABEL
Jun 10, 2025
PureTek Corporation
DUNS: 785961046
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Lidocaine HCl, Benzalkonium Chloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (31)
Drug Labeling Information
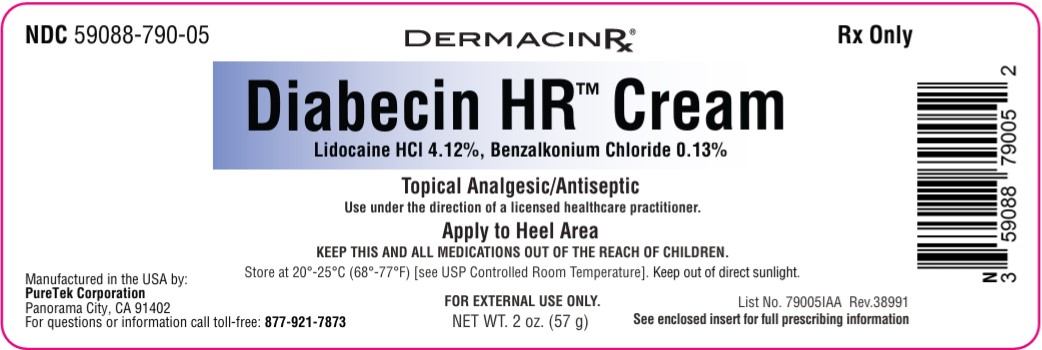
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Diabecin HR™ Cream
Manufactured by:
PureTek Corporation
Panorama City, CA 91402
For questions or information
call toll-free:877-921-7873
INDICATIONS & USAGE SECTION
INDICATIONS:
Diabecin HR™ Cream is indicated for the temporary relief of pain and itching associated with minor skin irritations. It combines the anesthetic properties of Lidocaine, and the antiseptic effects of Benzalkonium Chloride to provide effective care for damaged skin.
CONTRAINDICATIONS SECTION
CONTRAINDICATIONS:
Tuberculosis or fungal lesions of the skin vaccinia, varicella and acute herpes simplex and in persons who have shown hypersensitivity to any of its components. Lidocaine is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type.
WARNINGS AND PRECAUTIONS SECTION
WARNINGS: For external use only. Not for ophthalmic use.
EXCESSIVE DOSING:
Excessive dosing by applying** Diabecin HR™ Cream**to larger areas or for
longer than the recommended wearing time could result in increased absorption
of lidocaine and high blood concentrations, leading to serious adverse effects
(see ADVERSE REACTIONS, Systemic Reactions). Lidocaine toxicity could be
expected at lidocaine blood concentrations above 5 mcg/mL. The blood
concentration of lidocaine is determined by the rate of systemic absorption
and elimination. Longer duration of application, application of more than the
recommended number of patches, smaller patients, or impaired elimination may
all contribute to increasing the blood concentration of lidocaine. With
recommended dosing, the average peak blood concentration is about 0.13 mcg/
mL, but concentrations higher than 0.25 mcg/mL have been observed in some
individuals.
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS:
Application Site Reactions
Even though adverse reactions are rare, a very small percentage of patients experience an unpleasant burning sensation, redness, warmth, or stinging. It is advisable to apply a small amount on the forearm prior to first use. If any of these effects persist or worsen, contact your physician or pharmacist immediately. Systemic absorption of this medication is expected to be minimal when used as directed. However, if serious side effects occur (e.g., rash, swelling, severe dizziness), discontinue use and consult your pharmacist or physician. This is not a complete list of all possible side effects. You may report side effects to the FDA at 800-FDA-1088 or at http://www.fda.gov/medwatch.
Allergic Reactions:
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can occur. They are characterized by angioedema, bronchospasm, dermatitis, dyspnea, hypersensitivity, laryngospasm, pruritus, shock, and urticaria. If they occur, they should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
Other Adverse Events:
Due to the nature and limitation of spontaneous reports in post marketing surveillance, causality has not been established for additional reported adverse events including: Asthenia, confusion, disorientation, dizziness, headache, hyperesthesia, hypoesthesia, lightheadedness, metallic taste, nausea, nervousness, pain exacerbated, paresthesia, somnolence, taste alteration, vomiting, visual disturbances such as blurred vision, flushing, tinnitus, and tremor.
Systemic (Dose-Related) Reactions:
Systemic adverse reactions following appropriate use of lidocaine is unlikely, due to the small dose absorbed (see CLINICAL PHARMACOLOGY, Pharmacokinetics). Systemic adverse effects of lidocaine are similar in nature to those observed with other amide local anesthetic agents, including CNS excitation and/or depression (light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest). Excitatory CNS reactions may be brief or not occur at all, in which case the first manifestation may be drowsiness merging into unconsciousness. Cardiovascular manifestations may include bradycardia, hypotension and cardiovascular collapse leading to arrest.
To report SUSPECTED ADVERSE REACTIONS, contact Actavis at 1-800- 272-5525 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch for voluntary reporting of adverse reactions.
DRUG INTERACTIONS SECTION
Drug Interactions
Antiarrhythmic Drugs: Diabecin HR™ Creamshould be used with caution in patients receiving Class I antiarrhythmic drugs (such as tocainide and mexiletine) since the toxic effects are additive and potentially synergistic.
Local Anesthetics: When Diabecin HR™ Cream is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
CARCINOGENESIS & MUTAGENESIS & IMPAIRMENT OF FERTILITY SECTION
Carcinogenesis, Mutagenesis, Impairment of Fertility
**Carcinogenesis:**A minor metabolite, 2,6-xylidine, has been found to be carcinogenic in rats. The blood concentration of this metabolite is negligible following application of lidocaine.
**Mutagenesis:**Lidocaine HCl is not mutagenic in Salmonella/mammalian microsome test nor clastogenic in chromosome aberration assay with human lymphocytes and mouse micronucleus test.
**Impairment of Fertility:**The effect of lidocaine on fertility has not been studied.
DESCRIPTION SECTION
Full Prescribing Information:
Description:
Diabecin HR™ Cream contains 41.2 mg of Lidocaine HCl per gram, and 1.3 mg of Benzalkonium Chloride per gram in a vehicle of Aloe Barbadensis (Aloe Vera) Leaf Juice Powder, Aqua (Purified Water), Arnica Montana Flower Extract, Butyrospermum Parkii (Shea) Butter, Calendula Officinalis Flower Extract, Carbomer, Cetyl Alcohol, Chamomilla Recutita (Matricaria) Flower Extract, Cyclopentasiloxane, Dimethicone, Disodium EDTA, DL-alpha Tocopheryl Acetate, GenRx® Complex (Proprietary Blend), Glycerin, Glyceryl Acrylate/Acrylic Acid Copolymer, Glyceryl Stearate, Helianthus Annuus (Sunflower) Seed Oil, Methylsilanol Mannuronate, Panthenol, PEG-100 Stearate, Peucedanum Ostruthium (Masterwort) Leaf Extract, Phenoxyethanol, Propylene Glycol, Retinyl Palmitate, Sodium Lauroyl Sarcosinate, Stearic Acid, Tetrahexyldecyl Ascorbate, Triethanolamine, Vitis Vinifera (Grape) Seed Extract, Xanthan Gum, Zea Mays (Corn) Starch.
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY:
Pharmacodynamics
Lidocaine- is a common local anesthetic that relieves itching, burning, and pain. Topically, it blocks both initiation and conduction or nerve impulses by decreasing ionic flux through the neuronal membrane. Since it penetrates the skin, it creates an anesthetic effect by not just preventing pain signals from propagating to the brain out by stopping them before they begin. Benzalkonium Chloride serves as an antiseptic, preventing infection in minor skin injuries.
Pharmacokinetics
Absorption:
Lidocaine- Lidocaine may be absorbed following topical administration to mucous membranes, its rate and extent of absorption depending upon the specific site of application, duration of exposure, concentration and total dosage. In general, the rate of absorption of local anesthetic agents following topical application occurs most rapidly after intratracheal administration. Lidocaine is also well-absorbed from the gastrointestinal tract, but little intact drug appears in the circulation because of biotransformation in the liver. Lidocaine is metabolized rapidly by the liver and metabolites and unchanged drug are excreted by the kidneys. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/ toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine. Approximately 90% of lidocaine administered is excreted in the form of various metabolites and less than 10% is excreted unchanged. The primary metabolite in urine is a conjugate of 4-hydroxy-2, 6-dimethylaniline. The plasma binding of lidocaine is dependent on drug concentration and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 g of free base per mL, 60 to 80 percent of lidocaine is protein bound. Binding is also dependent on the plasma concentration of the alpha-1-acid glycoprotein. Lidocaine crosses the blood-brain and placental barriers, presumably by passive diffusion. Studies of lidocaine metabolism following intravenous bolus injections have shown that the elimination half-life of this agent is typically 1.5 to 2 hours. Because of the rapid rate at which lidocaine is metabolized, any condition that affects liver function may alter lidocaine kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction. Renal dysfunction does not affect lidocaine kinetics but may increase the accumulation of metabolites. Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6 g free base per mL. In the rhesus monkey, arterial blood levels of 18-21 g/mL have been shown to be threshold for convulsive activity.
Benzalkonium Chloride acts locally with minimal systemic absorption.
Excretion:
Lidocaine- Lidocaine and its metabolites are excreted by the kidneys. Less than 10% of Lidocaine is excreted unchanged. The half-life of lidocaine elimination from the plasma following IV administration is 81 to 149 minutes (mean 107 ± 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min (mean 0.64 ± 0.18 SD, n = 15).
Benzalkonium chloride, a quaternary ammonium compound, is also minimally absorbed through the skin when applied topically. If some systemic absorption occurs, benzalkonium chloride is metabolized in the liver and the metabolites are primarily excreted via the kidneys into the urine. The small amount absorbed is eliminated relatively quickly, reducing the potential for systemic toxicity.
PRECAUTIONS SECTION
PRECAUTIONS:
Allergic Reactions: Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine. However,** Diabecin HR™ Cream** should be used with caution in patients with a history of drug sensitivities, especially if the etiologic agent is uncertain.
Non-intact Skin: Application to broken or inflamed skin, although not tested, may result in higher blood concentrations of lidocaine from increased absorption.Diabecin HR™ Cream is only recommended for use on intact skin.
External Heat Sources: Placement of external heat sources, such as heating pads or electric blankets, overDiabecin HR™ Cream is not recommended as this has not been evaluated and may increase plasma lidocaine levels.
Eye Exposure: The contact ofDiabecin HR™ Cream with eyes, although not studied, should be avoided based on the f indings of severe eye irritation with the use of similar products in animals. If eye contact occurs, immediately wash out the eye with water or saline and protect the eye until sensation returns.
PREGNANCY SECTION
Pregnancy
Teratogenic Effects: Pregnancy Category B. Lidocaine has not been studied in pregnancy. Reproduction studies with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously and have revealed no evidence of harm to the fetus due to lidocaine. There are, however, no adequate and well- controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, lidocaine should be used during pregnancy only if clearly needed.
Labor and Delivery: Lidocaine has not been studied in labor and delivery. Lidocaine is not contraindicated in labor and delivery. Should lidocaine be used concomitantly with other products containing lidocaine, total doses contributed by all formulations must be considered.
Nursing Mothers: Lidocaine has not been studied in nursing mothers. Lidocaine is excreted in human milk, and the milk: plasma ratio of lidocaine is 0.4. Caution should be exercised when lidocaine is administered to a nursing woman.
**Pediatric Use:**Safety and effectiveness in pediatric patients have not been established.
OVERDOSAGE SECTION
OVERDOSAGE:
Lidocaine overdose from cutaneous absorption is rare but could occur. If there is any suspicion of lidocaine overdose (see ADVERSE REACTIONS, Systemic Reactions), drug blood concentration should be checked. The management of overdose includes close monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible value in the treatment of acute overdose with lidocaine.
In the absence of massive topical overdose or oral ingestion, evaluation of symptoms of toxicity should include consideration of other etiologies for the clinical effects, or over dosage from other sources of lidocaine or other local anesthetics. The oral LD50 of lidocaine HCl is 459 (346 to 773) mg/kg (as the salt) in non-fasted female rats and 214 (159 to 324) mg/kg (as the salt) in fasted female rats, which are equivalent to roughly 4000 mg and 2000 mg, respectively, in a 60 to 70 kg man based on the equivalent surface area dosage conversion factors between species.
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION:
Apply to the affected area of the heel two or three times daily or as directed by a licensed healthcare practitioner.
Use under the direction of a licensed healthcare practitioner.
HOW SUPPLIED SECTION
HOW SUPPLIED:
Diabecin HR™ Cream is supplied in a 2 oz (57 g) tube (NDC 59088-790-05).
CAUTION: KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
